Not long ago, we told you about a patient who received a stem cell treatment for degenerative eye disease. In that story, researchers took the patient’s skin cells and turned them into induced pluripotent stem (iPS) cells that were then made into retinal cells for transplantation.
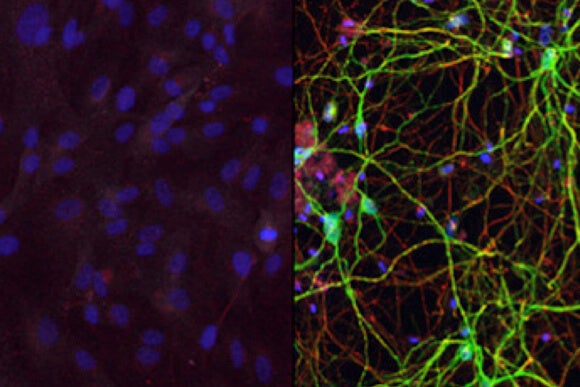
Now, researchers from Washington University in St. Louis have successfully skipped the intermediate stem cell stage and directly produced neurons from skin cells. While this study, published last week in the journal Neuron, was conducted in mice, it provides important evidence that this treatment option could be feasible for humans in the future.
The scientists, led by Dr. Andrew Yoo, were interested in producing a particular type of brain cell known as medium spiny neurons. These are the cells most affected by Huntington’s disease, a neurodegenerative disease that results in the gradual loss of muscle coordination and cognitive ability. Almost all people affected by the disease succumb to it within 20 years after the onset of symptoms.
After the discovery of iPS cells in 2006, many researchers attempted to skip the stem cell stage altogether in the hopes of producing whatever type of cell is needed.
Varying levels of success have been reported in the scientific literature since then, first using mouse cells and then human cells. Scientists have created a few types of neurons using this approach, including oligodendroglial cells, which are affected by multiple sclerosis and dopaminergic neurons, which are destroyed by Parkinson’s disease.
Now, Dr. Yoo’s group has gone beyond just producing these cells and has successfully transplanted them into mice. During the months following transplantation, they found that the neurons behaved exactly as if they were native cells, growing and making connections to other parts of the brain.
To change the skin cells into neurons, the scientists used two microRNAs called miR-9 and miR-124. As the name implies, microRNAs are small pieces of non-coding RNA that have been found to be important regulators of gene expression. Unlike messenger RNA (mRNA) which is the intermediate molecular step between DNA and protein synthesis, microRNAs help control which genes are expressed in which cells.
Since all of a person’s cells contain a full copy of their genome, the differences between various cells come only from which genes are expressed and which are silenced.
In this case, miR-9 and miR-124 were found to prime the skin cells to become neurons. To produce medium spiny neurons, a specific subtype of neuron, they next added proteins called transcription factors, which activated specific genes to coax the cells into the desired subtype.
Before transplanting the newly converted cells, the researchers subjected them to a battery of genetic and morphological tests to confirm they were indeed medium spiny neurons and not other types of neurons. The newborn cells passed their examination with flying colors.
Though this line of research is still considered to be in the early stages, it shows a great continuation of past successes by various research groups. It’s likely that longer-term studies are needed to see how the animals fare beyond just the six months reported in the paper.
Also, it is not yet clear if these cells can reverse the damage caused by Huntington’s disease because the cells were transplanted in healthy mice for this study. But Dr. Yoo and his team next plan to transplant the cells into a mouse model of the disease to see if they alleviate symptoms.
In the future, it will be interesting to see if other cells beyond neurons can be produced using a similar technique. Perhaps there will be a recipe book detailing exactly which microRNAs and transcription factors are needed to make each type of human cell.
Combined with the growing bioprinting industry, these and other techniques may lead to custom tissue made from a patient’s own cells, providing a near limitless supply to treat various illnesses.
Image Credit: Washington University in St. Louis, Jon Olav/Flickr



