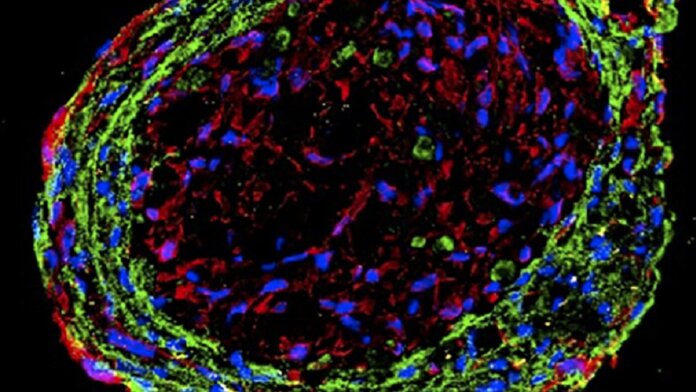
The tiny, floating blobs of mini-hearts were straight out of Frankenstein. Made from a mixture of human stem cells and a sprinkle of silicon nanowires, the cyborg heart organoids bizarrely pumped away as they grew inside Petri dishes.
When transplanted into rats with heart injuries they lost their spherical shape, spreading out into damaged regions and connecting with the hosts’ own heart cells. Within a month, the rats regained much of their heart function.
It’s not science fiction. A new study this month linked digital electrical components with biological cells into a cyborg organoid that, when transplanted into animal models of heart failure, melded with and repaired living, beating hearts.
At the heart (cough, pun intended) of the technology are electrically-active biodegradable silicon nanowires. Heart cells synchronize their movement to the beat of electrical activity, producing the standard “ba-bump, ba-bump” rhythm. A dose of nanowires into the organoids acted as a conductor to the symphony, allowing the lab-grown mini-hearts to better synchronize with their hosts.
Compared to standard heart organoids—grown exactly the same way but without the nanowire boost—the cyborg ones could better tolerate the hostile chemical environment inside the heart after a heart attack. They also better connected to their hosts during recovery, fighting off a detrimental side effect often seen after heart injuries.
For now the cyborg heart organoid transplant only works in rats. But it’s just a start.
Heartstopper
The heart is a trooper. From birth to death, it diligently contracts and releases to pump out blood full of oxygen to the rest of the body. It’s a biological wonder, faithfully lasting over 100 years in centenarians—far longer than most man-made hardware contraptions.
Yet the heart is also a failure point. Heart disease is the leading cause of death worldwide. A main reason is that cardiomyocytes—the “muscle cells” of the heart that contract—have very limited ability to regenerate. When damaged from a heart attack, scar tissue gradually grows around the injured areas, eventually limiting the heart’s ability to contract.
Scientists have long sought to treat heart disease with new, healthy cells. One popular idea is to guide human stem cells to develop into replacement cardiomyocytes. The lab-made heart muscle cells are then injected into damaged areas. Scientist have tested the treatment in a range of animal models of heart disease, including rodents, pigs, and nonhuman primates. But the healthy cells, when confronted with a hostile environment, struggled to survive. Those that did couldn’t reliably recover from heart damage, leading to potential problems with arrhythmia—irregular heartbeats that occur when different portions of the heart can’t beat in a synchronized rhythm.
Enter organoids. These structures loosely mimic their original counterparts in both their genes and diverse cell types. Grown inside lab dishes, the 3D blobs of tissue are widely used as surrogate organs to test new drugs or advance theories on how things work inside the body—for example, how to repair damage from a heart attack. But they also hold the potential to replace damaged tissue—something that’s already being explored for brain injuries.
Would it also work for the heart?
Back in 2017, the team envisioned a mini-heart—called a cardiac organoid—that combined a stew of different cell types. When churned inside a nutritious recipe “soup,” the cells organized into mini-heart organoids, such as a network of blood vessels that help carry oxygen. Yet a key component was missing: synchrony. Like a talented orchestra without a conductor, the resulting mini-hearts needed a “pulse” to keep the beat in tune.
Enter nanowires. Imagine them as rough, short hair you shave off. These strands of technological magic are made of silicon that conducts electricity. Compared to previous gold- or carbon-based nanowires, they are far more biocompatible and dissolve inside the body.
Roughly a decade ago, the team surprisingly found that the nanowires (called e-SiNW) can trigger human cardiomyocytes derived from stem cells to incorporate them as the cells develop into tiny blobs. Adding a dose of silicon made the resulting mini-hearts stronger, allowing the engineered organoid cells to pulse to the heart’s electrical tune.
Heart Broken
As a first test, the team directly injected the nanowires into the hearts of healthy rats. 28 days later (no it’s not that kind of zombie story), the rats went about their happy ways, meaning that the nanowires were biocompatible and safe.
Next, they made a “meatball” with roughly 1,000 human-derived heart cells and a similar number of nanowires, with a hefty dose of supporting cells added 10 days later. The mini-heart began pulsing inside a Petri dish in just seven days.
When transplanted into healthy rats, the cyborg meatballs slowly shredded their spherical shape, suggesting that they were integrating into the host’s heart environment. In less than a month, the mini-hearts—with their nanowires—formed multiple electrical connections with the host’s natural heart cells.
It shows that the nanowired organoids can hook up with a beating heart using electricity and blood vessels, said the team.
Then came the ultimate test: repairing issues after a heart attack. Here, the heart struggles to recover from a lack of blood and oxygen, often because of a blockage such as a blood clot. Once the blockage is cleared, blood rushes through the veins and often causes even more damage. A major hub is the left ventricle in the heart—the top-left portion of the organ. This is the “engine” of the body, pumping out blood to support the rest of the tissues. It’s also one that’s easily damaged in heart disease and generates a hostile local environment for new transplants. (Imagine trying to plant new trees inside an active volcano that just blew up.)
In one test, the team directly injected cyborg organoids and their purely biological counterparts into rats four days after a heart attack. Both grafts associated with their hosts just a week after transplant. The nanowired organoids meshed with the host hearts at a far higher level even around heavily damaged areas with scar tissue.
It’s a sign of their “capacity to survive in the most hostile regions” of the damaged heart, said the team.
Rats given the cyborg implants restored far more functionality than organoids without the nanowires. The rebuild extended beyond just the heart itself to help control blood pressure. By restoring a smooth flow of blood, the transplant “augments the therapeutic efficacy” of human mini-hearts, said the team.
The nanowires also endeared the mini-hearts to their hosts. 28 days after treatment, the hosts’ hearts had far less scar tissue that’s normally associated with heart failure. The cyborg transplants played nice with the rats’ immune systems, which usually ramp up after a heart attack. The main immune cells involved in the process are macrophages. These cells can be either devils or angels, triggering deadly immune responses or supporting restoration. Compared to unwired organoids, the cyborg ones bumped up the portion of “angel” immune cells in the graft and border zones to help mend the broken heart’s function.
There’s a long road to go before the results translate to humans. However, the results are the latest creative push for using organoids to patch up damaged organs. The “therapeutic synergy” between electrical nanomaterial and human mini-organs isn’t limited to the heart. A similar strategy could be used for other electrically active tissues such as the muscle or the brain, said the authors.
Image Credit: Tan et al/Science Advances