The Associated Press wire is all abuzz with the success of a recently completed trial to find a vaccine for HIV/AIDS. The 16,000+ person study, performed in Thailand by the US Army, the National Institute of Allergy and Infectious Diseases, and the Thai government, found that a new vaccine cocktail was able to reduce infection rates by 31%. The vaccine was a combination of two previously failed vaccines: ALVAC and AIDSVAX. While 31% is a far cry from the 100% success rate that we’ve all been hoping for, the trial does show that a useful HIV/AIDS vaccination system does exist for Southeast Asian strains of the disease. The trial will be presented and discussed at the AIDS Vaccine conference in Paris in October.
Trying to put the vaccine in context seems almost futile. You likely already know that more than 2 million died from AIDS in 2007, that thousands are infected every day and that a vaccine could save millions of lives and radically change the landscape of countries ravaged by the epidemic. In the world of HIV/AIDS, even a small hope for vaccination is a cause for celebration. What we have in the Thai study is likely a medium sized hope.
As discussed in the US Army factsheet for these trials, the reason Thailand was the focus of the study is that the Army has detailed data on the particular strains of HIV/AIDS seen in the region. While there is reasonable expectation that ALVAC/AIDSVAX combinations could work in other areas, their effect on different strains of the HIV virus is currently unknown.
Over 16,000 uninfected persons were used in the study. Of course, these people were not given the HIV virus. Instead they were given condoms, information on how to avoid infection, and regular examinations. Half received four ALVAC precursor shots followed by two AIDSVAX booster shots over six months, the rest were given placebos. Patients were followed for three years after their shots and those that developed HIV were given free antiviral medications.
As all of the 16,000+ were at medium risk to contract HIV in their daily lives, some did. 74 of those receiving placebo shots became infected, versus just 51 of the vaccinated. While that 31% difference is significant, 51 and 74 are small numbers compared to the thousands in the study as a whole. This has led to some criticism of the study based on statistical margins for error.
Also disappointing, but not specific to these trials, is the vaccines inability to affect the levels of HIV in blood of those infected. Researchers had hoped that an effective vaccination solution would also lower HIV proliferation in the body. The fact that the vaccine does not seem to affect individuals once they are infected suggests that scientists still do not fully understand the mechanisms for immunization.
As exciting as the Thai study is, this is not THE CURE for HIV/AIDS. Instead, it is a fairly effective vaccination, perhaps the only real one to date. The combination approach to creating a vaccine gives hope that the work previously done with ALVAC, AIDSVAX and other vaccine attempts will not have been in vain.
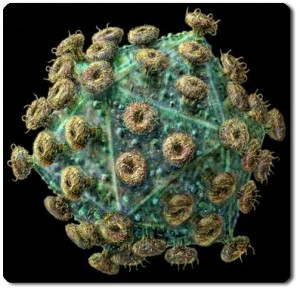
We can also be enthusiastic about the different ways that vaccines could function. ALVAC uses canary pox to introduce some HIV genes, AIDSVAX promotes the body to react to a HIV surface protein. Neither uses an actual HIV virion, nor can they cause infection. As genetic engineers, stem cell researchers, and nanotechnology experts progress in their fields, we could see wider and more varied combinations in the search for a 100% effective vaccine. The vaccine is coming, but for now, a vaccine is still pretty damn good.



