The blind really are beginning to see again. After receiving retinal implants in a trial, two people in the UK and one in China – all blind – regained part of their vision. And more good news could be on the way as results from other participants comes to light. But the chip is a bright ray of hope for the estimated 1.5 million worldwide that have retinitis pigmentosa, if not for the 285 million visually impaired.
All of the trial participants were made blind by retinitis pigmentosa in which the light-sensitive rods and cones of the retina deteriorate. British participants Robin Millar and Chris James, whose retinas had not responded to light in over a decade, were able to see immediately after the chip was turned on. Seeing the first flashes of light, James told the BBC, was a “magic moment.” Before receiving the implant neither participant was capable of detecting any light at all. The chip now allows James to distinguish between curves and straight lines. And Millar’s magic moment came when he began detecting light coming in through the windows. Professor Robert MacLaren, of Oxford Eye Hospital who co-led the study with Tim Jackson of King’s College Hospital, said the regained vision was a first for a completely blind Brit.
China scores its own first with Tsang Wu Suet Yun. Like James and Millar, Mrs. Tsang had lost her sight to retinitis pigmetnosa. She had been legally blind for 15 years, barely able to detect light. After receiving the same implant as James and Millar, she was able to read letters projected onto a screen.
The following is 2010 footage of a Finnish man who had regained partial vision after receiving an implant from Retina.
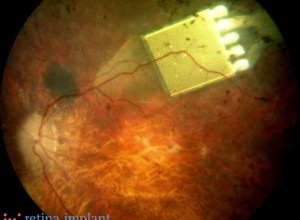
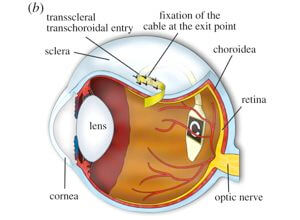
The implants act as a replacement for the lost retinal cells by detecting light and then stimulating neurons which send the signal to the brain. Developed by the world leader in retinal implants, Retina Implant Ag, the devices are tiny microchips 5 mm on each side and a tenth of a mm thick, which are implanted just below the retina. The chip’s surface is covered by a microphotodiode array containing 1,500 light-sensitive units. The light intensity of each point is translated into electrical impulses used to stimulate the underlying neurons. The chip is powered by a wireless power unit connected via a cable that runs over the ear and then under the skin to reach the eye. Settings on the power unit can be adjusted to modify the light sensitivity of the array and maximize its effectiveness for individual patients.
The implant has been involved in retinal trials for six years now, and the current encouraging results could be just the beginning. Results from the first two trials were published in 2010 and prompted the expansion of the trial to sites outside of Germany, including the UK and China.
Being able to distinguish between straight and curved lines or detecting light through a window may not sound like much but, as Prof. MacLaren points out, just being able to enter a room and know where the doors and tables would be is incredibly useful to a blind person. The vibrant colors of the world, however, will remain hidden for the moment. As the implants only convey light contrast they only see in black-and-white. But one unexpected development that’s as much a benefit to Millar as it is a neuroscience curiosity, he’s dreaming in color for the first time in 25 years.
It’s hard to tell without a direct comparison, but Retina’s chip has the potential to out-see the Argus II implant that is already commercially available and helping the blind to see. The Argus II chip doesn’t receive light directly, but relays signals from a glasses-mounted camera. And the chip only has about 60 electrodes with which to stimulate optic nerves and transmit the signal to the brain. Retina’s 1,500 adjustable, light sensing/nerve stimulating units could potentially work so much better.
To reiterate, the current results are part of a clinical trial and the chip is not yet available as a treatment. Replacing dead or non-functional cells with new ones through stem cell therapies would be the ideal treatment. While these therapies have shown great promise recently, there’s no telling just when they’ll deliver on restoring full vision to the blind, if ever. But the results from the current trial are just getting underway. Hopefully it will be more of the same.
[image credits: Retina Implant Ag and Proceedings of The Royal Society]
images: Retina Implant Ag, Royal Society
video: Retinal Implant Ag



