Nanotechnology Creates Artificial Artery for Clinical Trials

Share

Researchers at London Royal Free Hospital are hoping to save limbs and lives with the creation of their new artificial artery. Unlike current artery replacements, this grafting substance was created using nanotechnology and can pulse with the natural movements of the body. That pulsing will allow the polymer tube to be used in very small grafts (<8mm), giving hope that damaged arteries which would normally lead to amputations or heart attacks can now be treated. According to a recent press release, the Wellcome Trust has given [L]$500,000 to begin clinical trials of the new artificial arteries by the end of 2010. We could see the new polymer arteries in grafts, stints, and other vascular surgeries in the next few years.
Heart and vascular disease is the number one killer in most industrialized nations, and costs countries billions in health care, and lost wages. Nanotechnology, biotechnology, robotics, and stem cells are reinvigorating the development of artificial components of the cardiovascular system. We've seen hearts grown from stem cells in labs, artificial mechanical hearts, companies spending millions to develop artificial blood, and now even artificial vascular tubes which act more like the real thing. Combined with upcoming advances in robotic and micro-surgery, medicine could be on the path to conquering its public enemy number one.
The new artificial artery material was developed by Professors George Hamilton (vascular surgery) and Alexander Seifalian (nanotechnology and tissue repair). The substance is a polymer which has been embedded with different types of special molecules. Some of these molecules aid circulation, others encourage stem cells to coat its walls. That coating is very important and may allow the artificial tissue to bond better with the body and promote long term health. Most importantly though, the design of the artificial vascular tissue is resistant to clotting and can pulse.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Just those two traits put the new substance way ahead of current artificial arteries which have to be large in order to avoid dangerous platelet build up. In fact, for damaged arteries smaller than 8mm (~0.31 in), surgeons generally have to rely on finding donor veins in the patient's body. These veins are typically found in the lower limbs and surgically transplanted to where they are needed. When a patient doesn't have a good donor vein, and has artery damage that can't use a modern artificial graft...they can lose the limb with the damage, or are at very high risk for heart attacks (if the damage was located in the chest).
The Royal Free Hospital artificial artery then, is poised to fill a much needed gap in cardiovascular surgery devices and could save lives and limbs all over the world. Eventually, its developers hope to create an entire line of off-the-shelf grafts and stints to fit a wide-range of vascular needs. Hopefully the clinical trials in 2010 will prove very successful.
If they do, this will be another feather in the cap of nanotechnology, which has been slowly revolutionizing material sciences and will continue to do so in the upcoming years. Forget creating artificial arteries that are as good as the real thing, nanotech could make ones that are even better. Along with respirocytes (artificial blood cells), and medical nanobots, artificial vascular tissue is just one of the many ways that nanotechnology could extend the capabilities of the human body. Until we all get our new nanotech enhanced bods, we should probably keep in mind that the best way to survive heart and arterial disease is never to develop it in the first place. Stay healthy, everyone.
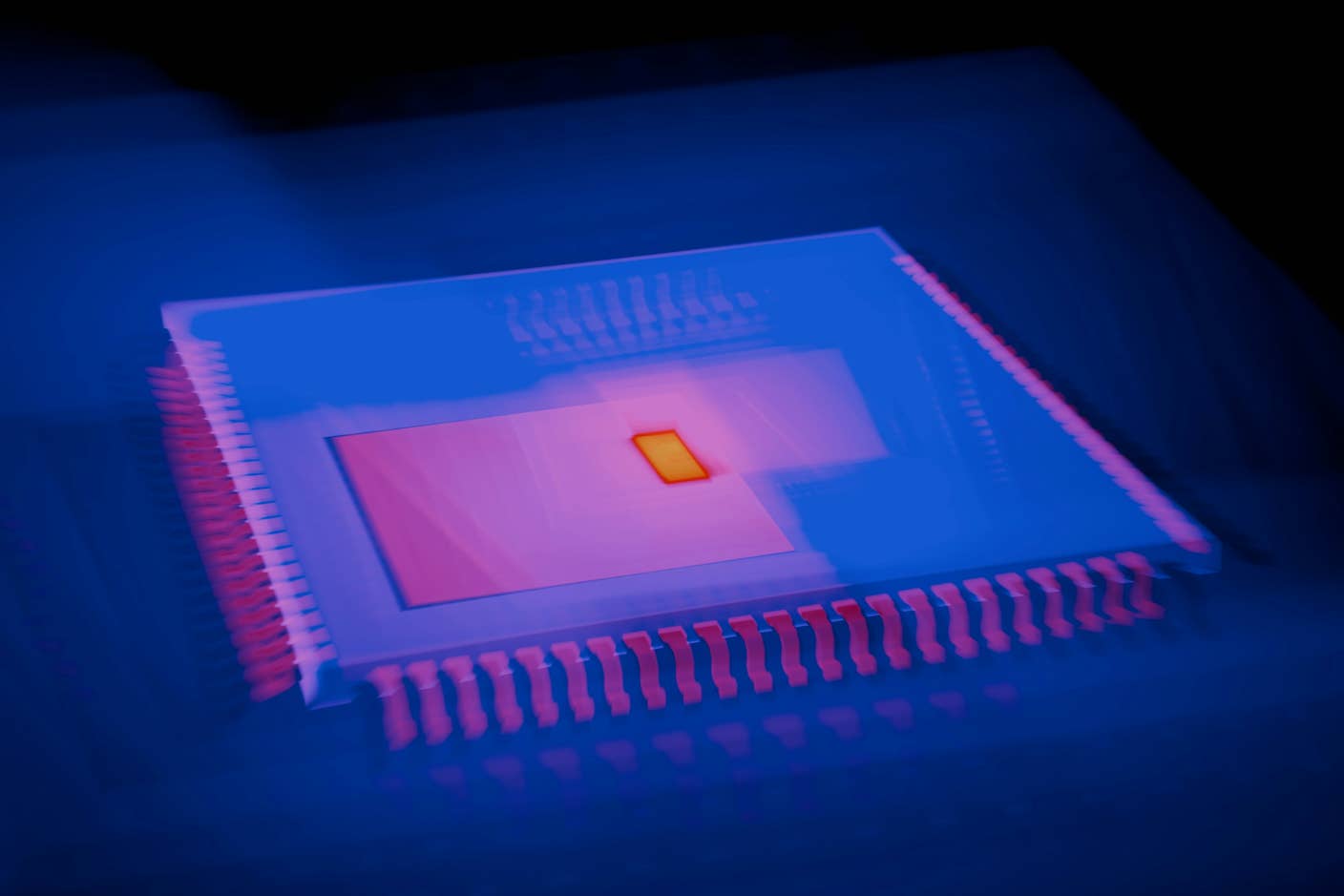
[photo credit: Royal Free Hospital, London]
Related Articles
This Light-Powered AI Chip Is 100x Faster Than a Top Nvidia GPU
This Week’s Awesome Tech Stories From Around the Web (Through December 20)
Data Centers in Space: Will 2027 Really Be the Year AI Goes to Orbit?
What we’re reading