Detecting Cancer Early With Nanosensors and a Urine Test

Share
How might cancer detection, treatment, and prevention change if cancer could be diagnosed by peeing in a cup?
According to Dr. Sangeeta Bhatia, about two-thirds of cancer deaths worldwide are probably preventable by techniques we already have in hand. Her laboratory is working to apply those techniques, and at Singularity University’s Exponential Medicine conference she shared details of an exciting project: using nanosensors to diagnose cancer with a urine test.
Bhatia is a professor at MIT’s Institute for Medical Engineering and Science and director of the Marble Center for Cancer Nanomedicine. She’s an affiliated faculty member of the Harvard Stem Cell Institute, an institute member of the Broad Institute, a biomedical engineer at the Brigham and Women's Hospital, and has been elected to Brown University’s Board of Trustees.
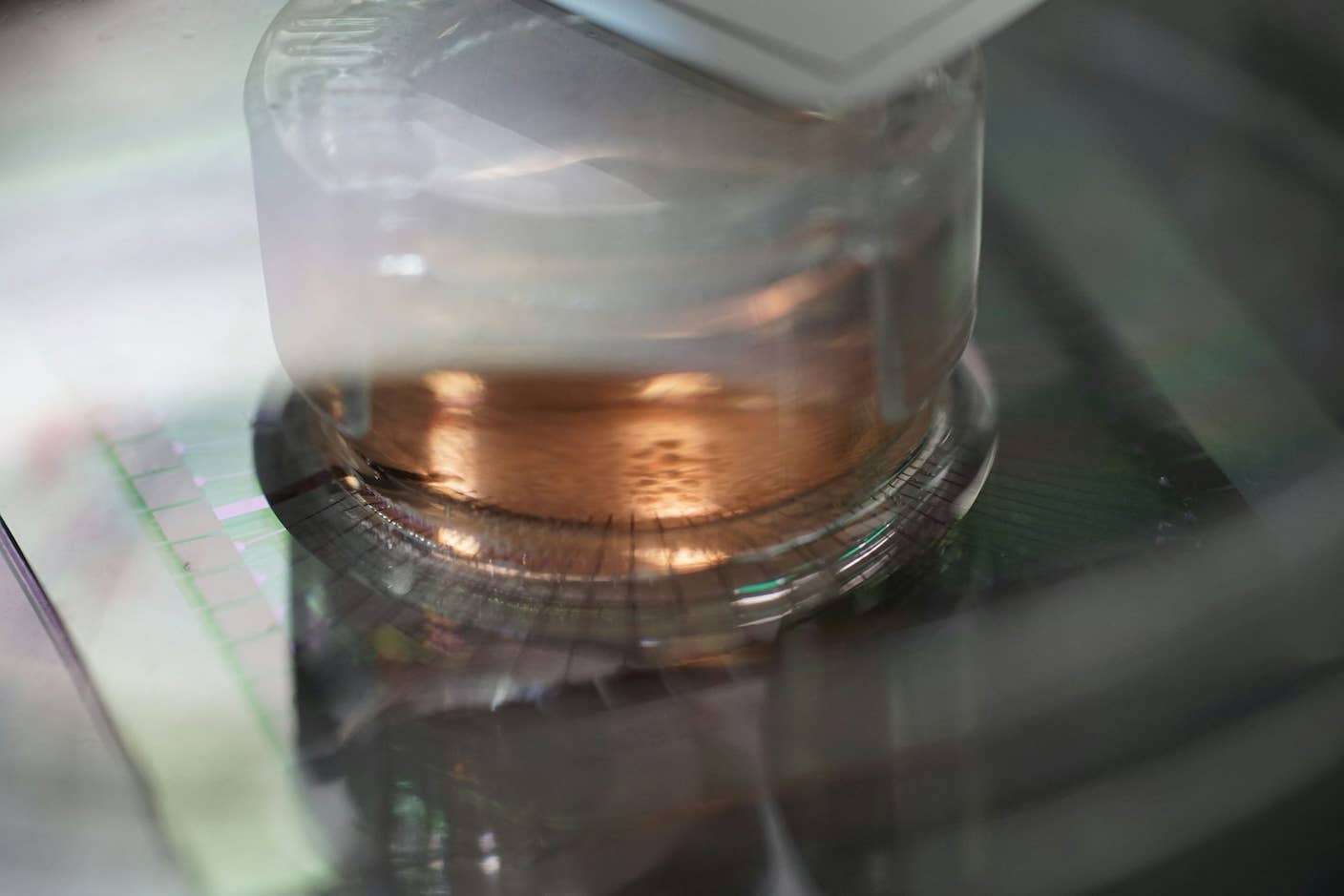
Trained as both a physician and an engineer, Bhatia’s laboratory is dedicated to leveraging miniaturization tools from the world of semiconductor manufacturing to impact human health.
Noting the remarkable pace of miniaturization and its power to impact medicine, Bhatia said a billion transistors now fit in the same space where just one used to fit, and the portability of computation has changed all of our lives.
Bhatia’s lab is interested in what the miniaturization revolution can do for cancer detection and therapy.
She predicted that by 2020, 70% of preventable cancer cases will be in the developing world. To meet the challenge of freeing millions of people from cancer, she said, “The way we think about detecting cancer and acting on it fundamentally needs to change.”
So how can miniaturization help?
Imagine a sensor so small it could circulate around the body, find cancer, then send a signal to the outside world. Bhatia thinks nanotechnology can get us there.
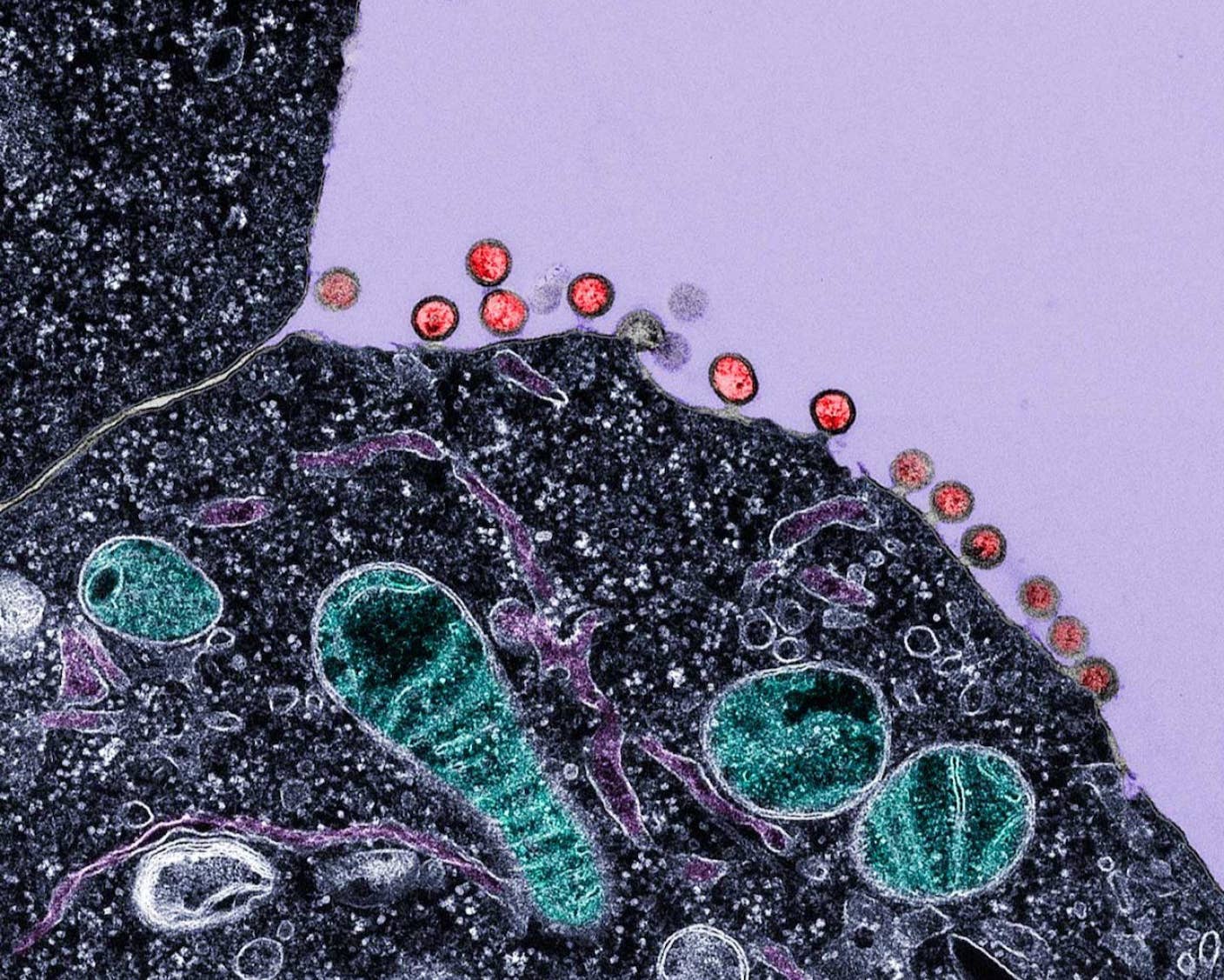
Hundred-nanometer particles (one thousand times smaller than the thickness of a human hair) are injected into a blood vessel. Thanks to their small size, the particles can ‘leak’ out of the blood vessel and into a cancerous tumor. The particles then detect enzymes that tumors make as they're invading.
The class of enzymes being detected are called endoproteases. There are over 500 of them in the genome, and they’re regulated through all the phases of cancer growth, including the immune response. Detectors can be made for any of these, and they have an important advantage: in traditional ultrasensitive cancer tests, higher specificity means less sensitivity, and vice versa. With nanosensors, multiple measurements can be taken at once. Bhatia refers to this as multiplexing.

Dr. Sangeeta Bhatia at Exponential Medicine.
Rather than just making one sensor against one enzyme, a cocktail of sensors can be made and pointed at different cancer targets or different phases of cancer. The most common test Bhatia’s lab uses is a tenplex, and every fragment that comes out in the urine is designed to detect a different enzyme.
Speaking of urine—the final step is getting this activated signal out of the body. Lucky for us, it turns out our kidneys are natural nanoscale filters, able to filter down to a five-nanometer scale.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


That means the whole process of detecting cancer by peeing in a cup would go like this: a hundred-nanometer particle is injected into the patient, where it leaks into the tumor, detects enzymes ultra-sensitively, and gives off a five-nanometer fragment which the body concentrates in urine.
There are other tests for cancer being developed for the blood and focusing on various cancer byproducts, such as fragments of mRNA. Whether it’s blood or urine tests, a tumor wouldn’t have to be located or biopsied. The hope is to better fight cancer by diagnosing it early when it’s more treatable.
But Bhatia’s approach may have an added benefit due to its prospective simplicity.
She emphasized her technology’s potential for use in the developing world. The method could be an inexpensive point-of-care test that won’t require steady electricity or an on-site physician. Patients will be able to get a shot, wait an hour, and do a urine test on a paper strip. They could then take a photo of the paper strip with a smartphone and send it to a physician or database.
While taking a test to find out whether you have cancer will never be a pleasant activity, it’s a plus that nanosensors may prove a viable alternative to blood tests, as well as detect cancer early enough to give patients a better chance of survival.
Of course, finding cancer is only half the battle. Bhatia also noted her team (and others) are aiming to better treat cancer by developing drug-loaded nanoparticles that seek and destroy cancer cells. Instead of a body-wide blast of toxic chemotherapy, more precisely targeted nanoparticle delivery would reduce dosage—and hopefully, nasty side effects—while increasing the efficacy of the drugs.
Work on nanoscale detection and treatment may help us fight cancer far more effectively in the future.
Want to keep up with coverage from Exponential Medicine? Get the latest insights here.
Image credit: Shutterstock
Vanessa has been writing about science and technology for eight years and was senior editor at SingularityHub. She's interested in biotechnology and genetic engineering, the nitty-gritty of the renewable energy transition, the roles technology and science play in geopolitics and international development, and countless other topics.
Related Articles

This Week’s Awesome Tech Stories From Around the Web (Through December 13)
New Immune Treatment May Suppress HIV—No Daily Pills Required
How Scientists Are Growing Computers From Human Brain Cells—and Why They Want to Keep Doing It
What we’re reading