Party Drug MDMA Inches Closer to Breakthrough Approval for PTSD

Share
MDMA doesn’t have the best reputation. Known as “ecstasy” or “molly,” the drug is synonymous with rave culture: all-night electronic beats and choreographed laser shows.
Still, it may soon join the psychedelic drug resurgence—not for partying, but for tackling severe mental trauma, such as post-traumatic stress disorder (PTSD).
Last week, Nature Medicine reported a multi-site, randomized, double-blind trial in over 100 patients with PTSD. The drug, combined with therapy, was carefully administered to patients being monitored in doctors’ offices. Compared to patients given the same therapy with a placebo, MDMA was far more effective at dampening PTSD symptoms.
The study, led by the non-profit Multidisciplinary Association for Psychedelic Studies (MAPS), follows an earlier Phase 3 trial—the last stage of clinical testing before regulatory approval. In that trial, participants also received therapy. Roughly twice the number of people given MDMA rather than a placebo recovered from their PTSD diagnosis.
The new, long-awaited study bolsters those earlier results by recruiting a more diverse population and showing that the treatment worked across multiple racial and ethnic groups.
To be very clear: the trials are for MDMA-assisted therapy. The psychotherapy component is key. The team repeatedly warns against seeking out the drug and taking it without supervision.
“What we believe is that the results that we got were not from MDMA,” said MAPS founder Rick Doblin to Nature in an earlier interview. “They were from highly trained therapists who are then using MDMA.”
The Food and Drug Administration generally requires two controlled trials before it considers approving a drug. MAPS has now delivered. The organization plans to seek approval this October. If the results hold up, the US may join Australia in welcoming a previously condemned drug as a new treatment for PTSD.
It won’t be an easy road. Although public and scientific opinions have shifted towards tolerance, MDMA is still listed as a Schedule 1 drug by the DEA. Drugs in this category are deemed to have “no currently accepted medical use and a high potential for abuse,” placing them alongside heroin.
That said, scientists are increasingly taking psychedelics seriously as tools that can help combat difficult mental problems. Also among Schedule 1 drugs are cannabis, psylocibin (from magic mushrooms), and LSD (commonly known as acid). These illicit drugs are gradually being embraced both in the research and clinical spheres as valid candidates for further study.
To Dr. Amy Kruse at the venture capital firm Satori Neuro based in Maryland, who was not involved in either study, “MAPS has been the beacon to kind of take on this work…There are many people that can benefit from this treatment, and I think it shows a pathway for the potential rescheduling of other molecules.”
A Checkered Past
MDMA—an acronym for its chemical name, 3,4-methylenedioxymethamphetamine—didn’t always wear the party drug black hat. It has enthralled psychiatrists since its birth in 1912.
Developed by a German pharmaceutical company to control bleeding, the drug soon caught the eye of mental health professionals. From the 1970s to its complete ban in 1985, thousands of individual reports suggested the drug, delivered in a doctor’s office with therapy, enhanced treatment results. Patients seemed to be able to better express and process their feelings, in turn gaining insights into their own mental states.
However, the drug also leaked out onto the street around the same time, spurring a total ban by the FDA in 1985. Research into its potential for enhancing psychotherapy screeched to a halt. In turn, scientists were left with only individual case reports and anecdotes—hardly sufficient evidence to continue research.
Enter Doblin. Convinced that research into MDMA and other psychedelic drugs shouldn’t be abandoned, he founded MAPS in 1986—a year after the ban. For the next 40 years, his team fought to reestablish the drug as a legitimate candidate for PTSD and depression. Neuroscientists studying drug toxicity was the norm. Treatment potential? Not so much.
Opinions began to shift in the late 2010s. A prominent neuroscientist called the drug “a probe and treatment for social behaviors” in a highly prestigious journal. MDMA regained its 1970s reputation as an “empathogen,” in that it fosters feelings of empathy and closeness. How MDMA triggers those intimate feelings isn’t yet fully understood, but it seems to increase levels of several chemical messengers in the brain, including serotonin, dopamine, and norepinephrine. Lower amounts of these chemicals are often associated with depression.
In 2021, MAPS and Doblin had their first major win in a clinical trial studying 90 people with PTSD undergoing therapy, either with MDMA or a placebo. After three sessions, 67 percent of those receiving MDMA no longer qualified for PTSD diagnosis, compared to just 32 percent of people given placebos.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


The new 104-person study bolsters these promising results. Patients attended three 8-hour sessions across roughly 12 weeks. Regardless of ethnicity or race, 71 percent of people given MDMA and therapy were freed of their PTSD diagnosis, compared to 48 percent in the placebo group. MDMA-assisted therapy was also effective in people with other mental disorders, such as depression—an important use case as the two conditions often go hand-in-hand. Most participants experienced mild side effects, such as muscle tightness, feeling hot, or nausea.
Neurologist Dr. Jennifer Mitchell at the University of California, San Francisco, who led both Phase 3 studies, told Nature that the drug acts as a “communications lubricant.” It doesn’t make therapy sessions more fun—participants still have to work through their trauma—but it does help them more readily open up to their therapists, without experiencing shame or trauma.
And these effects are seemingly generalized regardless of ethnicity or race. “In a historic first, to our knowledge, for psychedelic treatment studies, participants who identified as ethnically or racially diverse encompassed approximately half of the study sample,” the team wrote.
A Bright Future?
It’s extremely difficult to blind a psychedelic study. Given MDMA’s potent effects, it’s very clear to patients if they’re high after taking a pill, which could result in bias.
To get around the problem, MAPS developed a special protocol first approved by the FDA in 2017. After each treatment session, the volunteers’ symptoms were measured by psychologists not privy to the experiment design. They’re “blinded” to what group the patient is in and did not administer the drug or therapy.
It’s not a perfect solution. In a post-trial survey, most people given MDMA knew what they were given. To Dr. Erick Turner at the Oregon Health and Science University in Portland, this doesn’t fit the FDA’s definition of “blinding.” Even if the drug is deemed safe and efficient, regulatory agencies will still need to iron out the rules. Because therapy is a key component but not under the FDA’s jurisdiction, the agency has to somehow dissuade people from trying the drug on their own in inconducive, or even dangerous settings.
MDMA has also been linked to bad experiences in people with schizophrenia or other neurological disorders. These terrifying trips aren’t just detrimental to the patient’s mental health—they could also set back the renaissance of psychedelic treatments.
In all, lots of kinks need to be worked out. Given MDMA’s long history, its patent is expired, reducing incentives to develop or manufacture the drug. But with the new study, regulatory approval is inching closer as an alternative for people battling mental demons.
“It’s an important study,” said MDMA researcher Dr. Matthias Liechti at the University of Basel in Switzerland, who wasn’t involved in the trial. “It confirms MDMA works.”
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
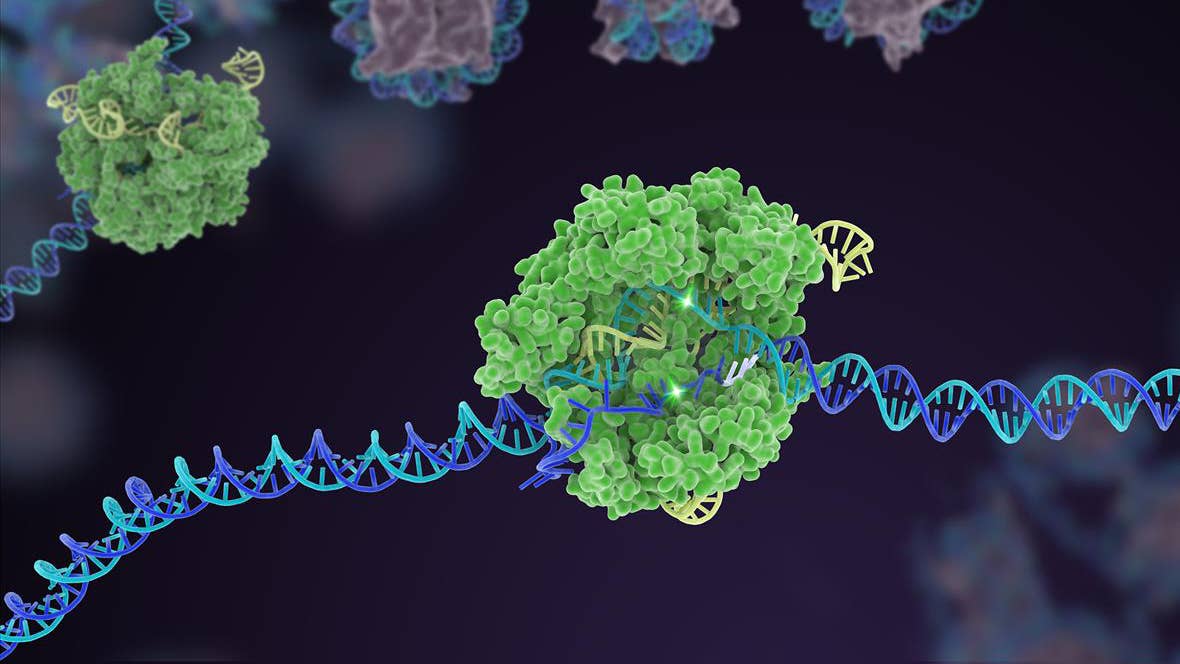
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

This Brain Pattern Could Signal the Moment Consciousness Slips Away
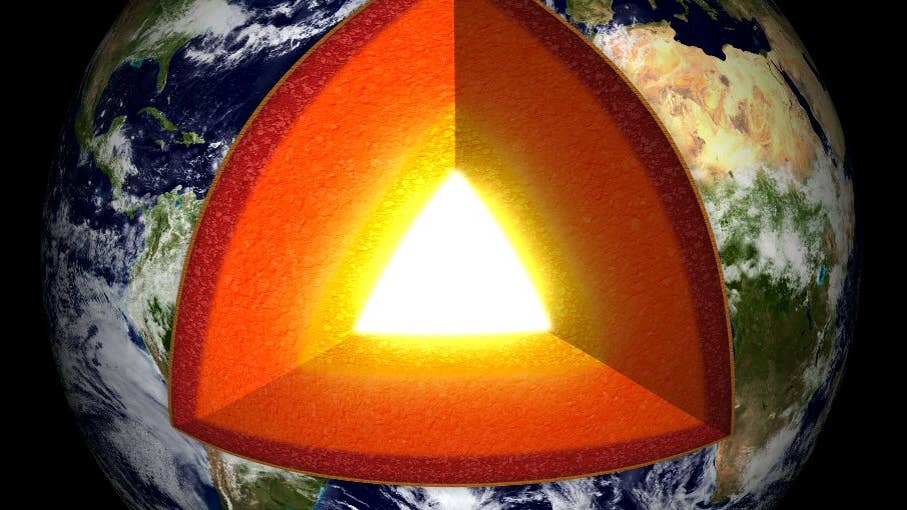
Vast ‘Blobs’ of Rock Have Stabilized Earth’s Magnetic Field for Hundreds of Millions of Years
What we’re reading
