After Weight Loss, Ozempic Is Set to Conquer a Universe of Brain Disorders
Share
One inescapable word dominated biomedicine this year: Ozempic.
Physicians were amazed at the drug’s efficacy in treating diabetes, for which it is FDA approved, and obesity. Social media propelled it into the year’s zeitgeist as a “miracle” weight-loss drug that can help people effortlessly shed pounds—for health or for vanity.
It’s no wonder. Diet pills have a long and tumultuous history. From amphetamine-laden “rainbow pills” to the notorious fen-phen and its deadly side effects in the lungs and heart, these pills have a killer reputation.
Scientists have long searched for a safe and effective pill that curbs appetite without dangerous consequences. Though it isn’t free of side effects, Ozempic comes much closer to fitting the bill. It works its magic by mimicking the body’s natural response after a satisfying meal—it makes the user feel full. Without having to resist constant hunger, the pounds melt away.
For many people struggling with obesity, the drug is a potential lifesaver. Excess weight is associated with higher incidences of stroke, heart and liver disease, sleep apnea, joint problems, and some cancers. A major clinical trial this year in tens of thousands of overweight people without diabetes found the main ingredient in Ozempic, semaglutide, reduced the risk of stroke and heart attack, while lowering the chances of death due to cardiovascular problems.
Perhaps even more importantly, the drug is gradually changing societal views on obesity—it’s not due to lack of will power, but a chronic medical condition that can be treated.
But Ozempic and similar drugs—like Wegovy, another semaglutide-based medication that has been FDA-approved for weight loss—are already set for the next chapter: tackling a wide range of brain disorders, including Alzheimer’s and Parkinson’s. Clinical trials are underway for addiction, and the drugs are showing early promise battling bipolar disorder and depression.
Gut to Brain
Why would drugs useful in the treatment of diabetes and weight loss also prove effective for mood, addiction, and neurodegenerative diseases?
It comes down to how Ozempic and Wegovy work. Both contain semaglutide, a chemical that mimics a hormone called glucagon-like peptide-1, or GLP-1. After a meal, as our gut senses an influx of nutrients, cells in the intestine release the hormone. GLP-1 tells the stomach to slow down how fast it’s emptying its contents. It also triggers the pancreas to release more insulin to keep blood sugar in check—maintaining a metabolic state that’s critical for brain health.
But here’s the crux. GLP-1 doesn’t just roam the gut; it also easily enters the brain.
Protected by a tight-knit cellular barrier, the brain often rejects large molecules that could damage its sensitive neurons, but it readily admits GLP-1. The hormone activates neurons in a wide range of brain areas, including the “reward center” and hippocampus, which play critical roles in the regulation of mood and memory.
This has neuroscientists wondering: Can GLP-1 tweak brain function to support neurological or mental health?
Addiction
One tantalizing side effect of people taking GLP-1-like drugs has been that they’re less interested in consuming alcohol and other mind-bending substances. Why this happens is unclear, but it’s likely because the hormone dampens reward pathways in the brain.
One study, for example, gave alcoholic monkeys (yup, that’s a thing) access to an open bar for four hours a day. These monkeys love their booze. Thriving in the Caribbean, they are notorious for swiping alcoholic drinks from tourists. After two to five weeks of treatment, those injected with GLP-1-like drugs reduced their alcohol intake even when tempted with all-you-can-drink alcohol. Instead, they readily slurped fresh water.
GLP-1 mimics may also help curb smoking addiction. A small clinical trial in 2021 found smokers, while wearing nicotine patches, readily kicked the habit when injected with a first-generation GLP-1 drug. Nearly half of the GLP-1 treated participants quit smoking—a success rate almost double that of a control group that only wore nicotine patches.
As with any new drug, the results aren’t cut and dried. One study for alcoholism using a first-generation GLP-1 mimic found little difference in people undergoing behavioral therapy. Both groups lowered their alcohol consumption, but the GLP-1 drug didn’t further bolster recovery. A trial using the drug for cocaine abuse also found negligible effects.
That said, semaglutide is far more efficient than first-generation GLP-1 mimics. Clinical trials are in the works, some using brain-imaging to see how the brain reacts to the drug in real time.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Mood Disorders
Depression and other mood disorders are also possible targets for GLP-1 mimics.
Often considered purely neurological, mood is tightly linked to other parts of the body, including the gut. People with depression often experience changes in appetite and gut hormone levels—including GLP-1.
An analysis of six trials with over 2,000 participants found GLP-1 mimicking drugs eased their depression. Another trial involving 29 people with bipolar disorder or depression found the drugs leveled mood swings for at least six months after treatment.
The drugs could work by changing neural connections in the brain.
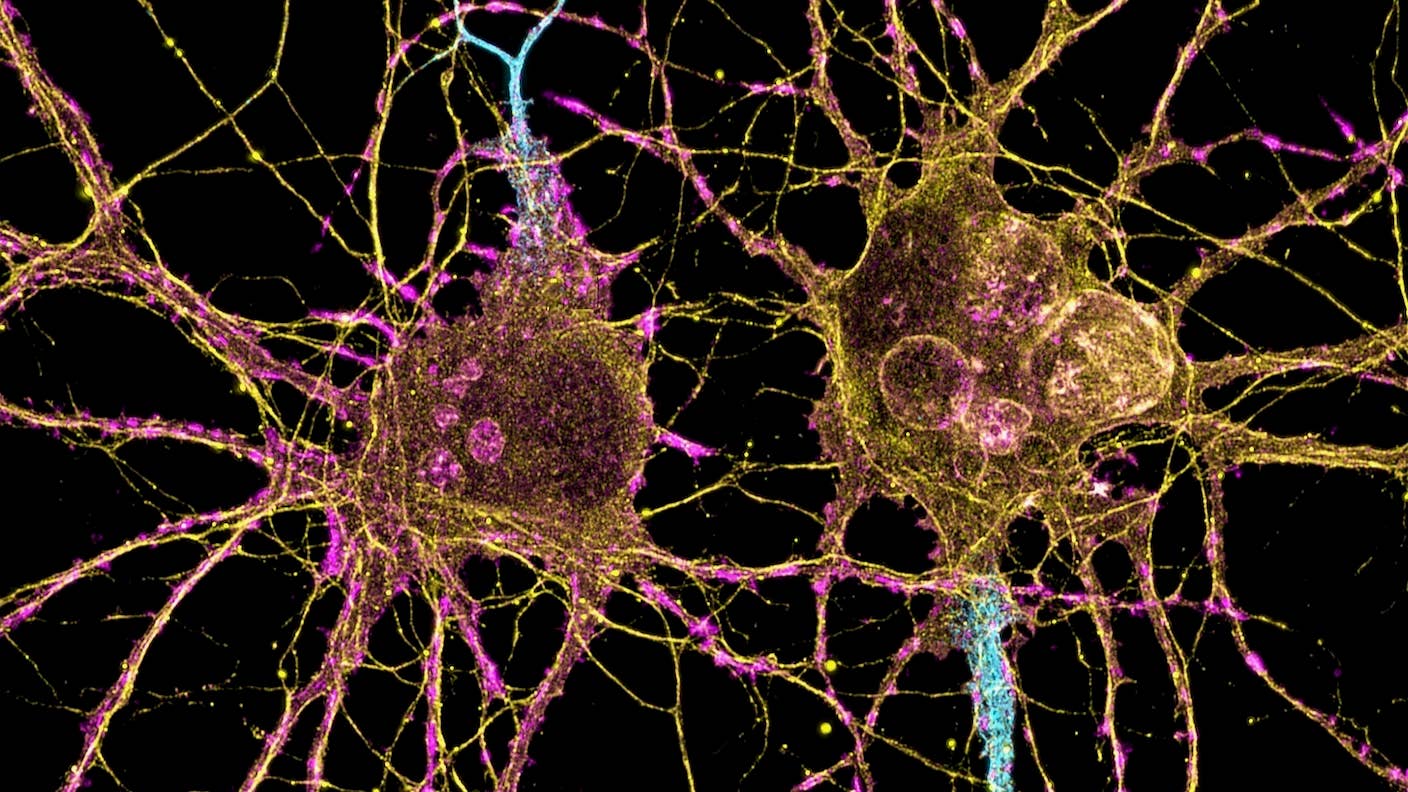
Neurons look a bit like trees, with giant trunks that process information and branches that “talk” to neighbors. These branches wither in a depressed brain, making it difficult for neurons to connect to each other and form healthy networks. What’s more, the hippocampus—a brain region critical to memory—struggles to birth new neurons, which help maintain memory and mood. All these changes contribute to mood disorders.
Classic antidepressants and newer therapies, including ketamine, reverse depressive symptoms by helping neurons regrow their branches. Initial studies in mice suggest GLP-1-like drugs also rewire brain regions that shrivel with depression and alleviate manic symptoms in bipolar mice. While still preliminary, these results pave the way for further testing in humans.
Alzheimer’s Disease
Dementia is a grueling journey for those suffering symptoms and their families. Neurodegenerative disorders, such as Alzheimer’s or Parkinson’s disease, slowly eat away at memories, reasoning, and eventually take lives. Chronic inflammation, which damages neurons and blood vessels and is linked to uncontrolled levels of blood sugar, is a major player.
Because Ozempic and similar drugs lower blood sugar, they could potentially also dampen inflammation in the Alzheimer’s brain and slow the loss of cognition. A few trials are in the works. Novo Nordisk, the Danish pharmaceutical giant behind Ozempic and Wegovy, launched two clinical trials in 2021 to see if semaglutide slows cognitive decline in Alzheimer’s patients. First results are expected in 2025. Meanwhile, multiple companies, including Neuraly and Kariya Pharmaceuticals, are testing whether GLP-1 mimicking drugs can restore cognition in Parkinson’s disease.
For now, we don’t fully understand how these drugs work in the brain. They could alter cholesterol metabolism—an essential process by which neurons build their protective sheaths. GLP-1 also reworks the way neurons connect with each other to form functional networks, which could be how Ozempic and similar drugs work in the brain.
Whether the effects last is another mystery. Early results for obesity suggest GLP-1 mimics aren’t “forever drugs,” in that the patients’ weight partly bounces back after discontinuing the daily regime. As for the brain? Only time will tell.
Image Credit: NIH
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles

Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading