Scientists Just Inched Closer to Lab-Made Human Eggs and Sperm
Share
We all know the drill for reproduction—sperm meets egg.
For the past decade, scientists have been pushing the boundaries of where the two halves come from. Thanks to induced pluripotent stem cell technology, it’s now possible to scrape skin cells from mice and transform them into functional sperm or egg cells that give rise to healthy pups born from two moms or dads. The recipe may even open the door for single parent offspring—at least for mice.
But mice aren’t people. And the same recipe doesn’t work for human reproductive cells.
One reason, according to Dr. Mitinori Saitou at Kyoto University, is due to the chemical “tags,” known collectively as the epigenome, that control when certain genes are turned on or off. Like a ledger, these tags maintain a sort of memory in early reproductive cells. For cells to eventually develop into sperm or eggs, those memories must be wiped clean.
This month, Saitou’s team developed a recipe to do just that. Starting from primordial germ cells—a type of cell that eventually develops into either sperm or egg—they added a single protein ingredient that nudged their growth further along by erasing their chemical memories.
“Our study represents…a fundamental advance in our understanding of human biology and the principles behind epigenetic reprogramming in humans,” Saitou said in a press release. It’s also “a true milestone” for generating sperm and eggs in the lab, he said, which could potentially help couples struggling with infertility.
Tag, You’re It
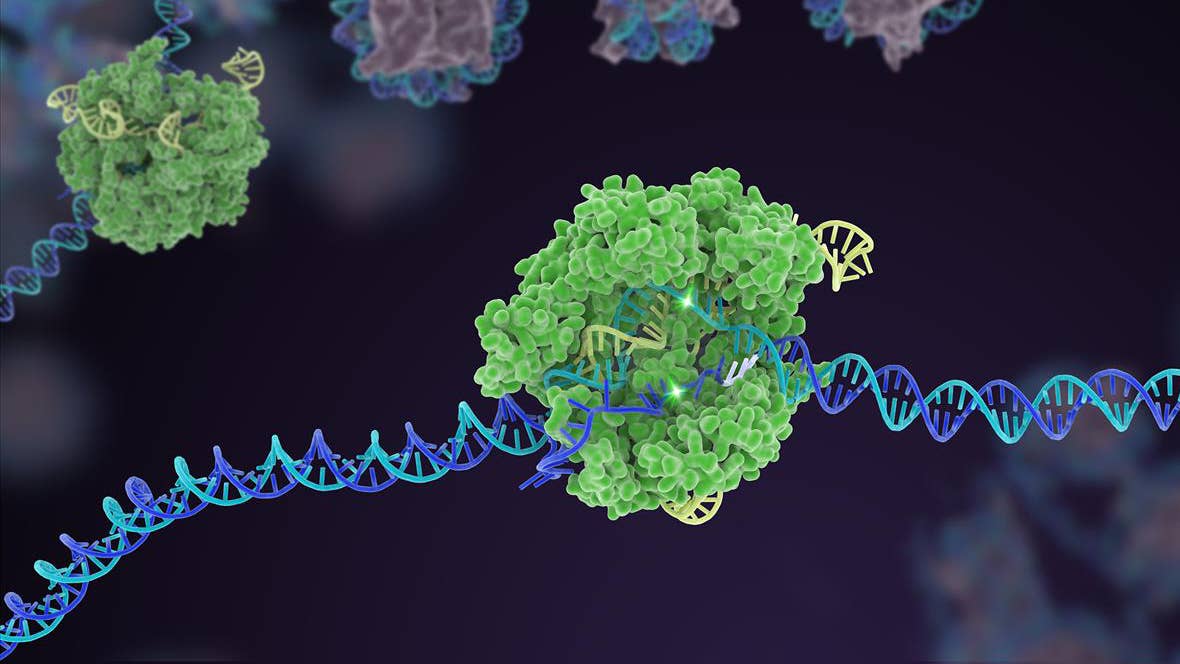
Epigenetic tags control how our genes are expressed. Picture DNA’s double helix. Then imagine sticking small chemical “pins” into the structure. These pins readily block the transcription of our genetic blueprint into biological messages—make this protein, not that.
It may sound nefarious, but epigenetic tags are fundamental to our bodies. Most of our cells have the same DNA—it’s the expression of that DNA that allows them to form different tissues and organs and guides biological processes. Depending on where, and which, tags are added to the double helix, some shut down entire genes—sometimes for life.
But epigenetics becomes a hurdle when growing gametes—egg or sperm cells—in a dish. Called in vitro gametogenesis, the technology allows scientists to take a closer look at how gametes develop and potentially help couples struggling with infertility.
It also offers a way to fix DNA that leads to inherited diseases, especially if only one parent has the mutation. Although scientist have edited genes directly in early human embryos using CRISPR-Cas9, the approach is prone to errors and can cause potentially dangerous side effects. Rewriting DNA in sperm and egg cells is simpler—the cells can readily repair DNA, a critical step in gene editing—and lab-grown specimens are the perfect canvas to experiment on.
The problem? Their epigenetic chemical tags form a sort of “memory,” which eventually causes them to stop developing. The body naturally wipes the tags away, a process dubbed epigenetic reprogramming, so that early reproductive cells can grow into healthy egg or sperm.
While scientists can already replicate the process in mice, the same recipe doesn’t work in human cells. Why this is so is still a mystery. In the new study, Saitou’s team set out to find an epigenetic “reset” button tailored to human reproductive cells.
One Protein to Rule Them All?
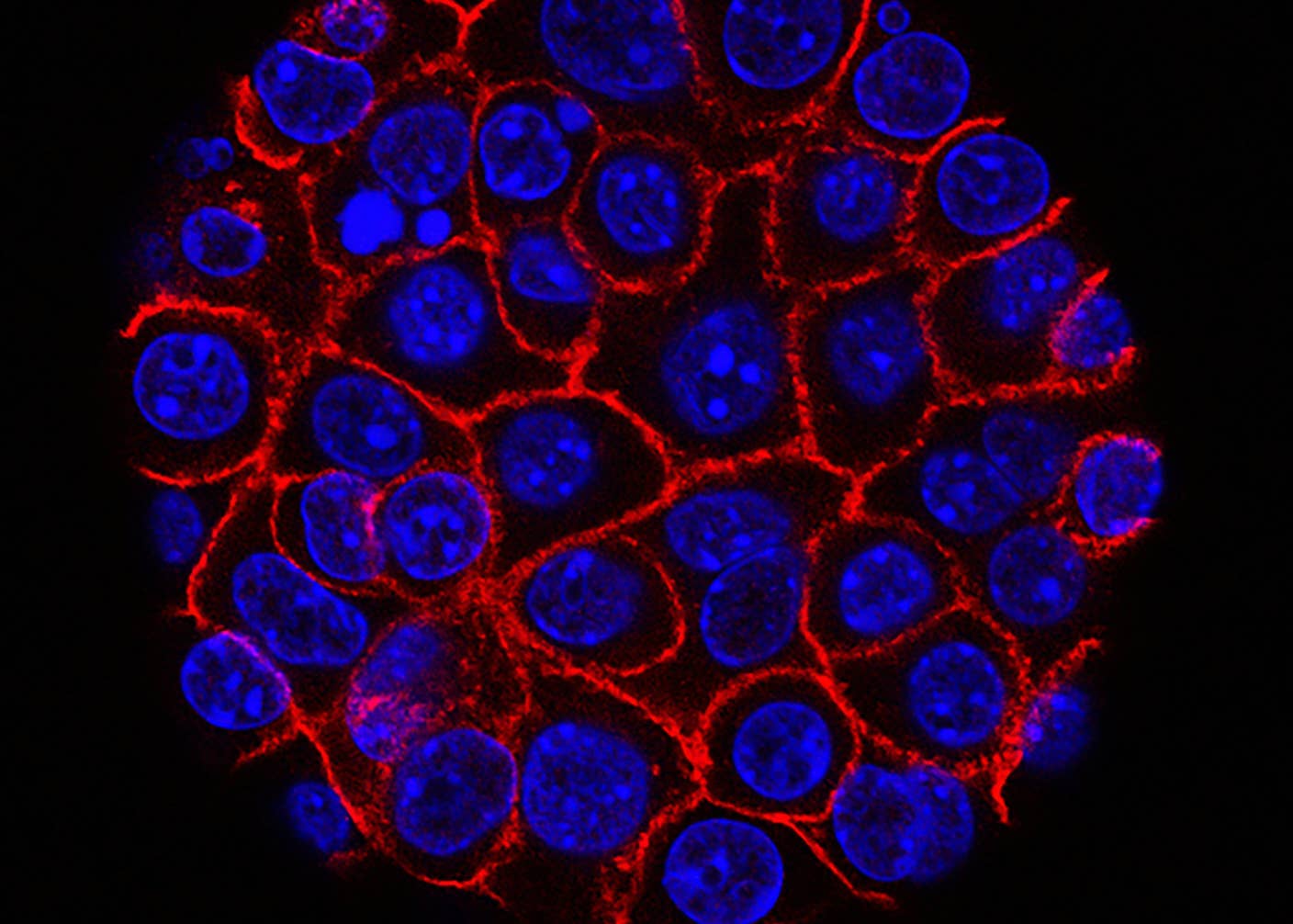
Saitou is hardly new to the field. Previously, his team coaxed stem cells into another type of cell that roughly resembled early reproductive cells. They recapitulated several fundamental characteristics of their natural counterpart—such as the capacity to rapidly multiply.
However, their epigenetic landscape remained intact, eventually halting the cells’ development. As a workaround, the team mixed them with mouse cells from reproductive regions in the body to mimic the microenvironment of the ovary or testis. It worked—molecular signals from the supporting cells eased off the epigenetic brake, allowing the lab-grown early reproductive cells to further develop into immature gametes that, in theory, could become egg and sperm.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


While successful in concept, the process was highly inefficient, with roughly one cell out of ten able to develop further. And mixing human cells with mouse cells could have unintended consequences, which isn’t ideal or practical for studying human reproduction. But the results sparked an idea: Some molecules could switch on epigenetic reprogramming in lab-grown early reproductive cells—they just needed to find them.
The new study homed in on one. Dubbed BMP2, the protein is familiar to scientists for its role in development—for example, forming bones and cartilage. But “it was highly unexpected that it also drives…epigenetic reprogramming,” said Saitou.
When added to lab-grown early reproductive cells, they developed further than previous attempts, forming precursors to human sperm and eggs inside a dish. The cells had a similar genetic and epigenetic profile to their natural counterparts and could rapidly proliferate—in some cases, over 10 billion-fold.
It’s “near-indefinite amplification…we now also have the ability to store and re-expand these cells as needed,” said Saitou.
However, even with BMP2, the treated cells couldn’t develop into fully mature sperm and eggs. Carefully analyzing the cell’s epigenome, the team found some epigenetic marks still remained—suggesting the reprogramming wasn’t complete.
While a headache for research, these epigenetic “stragglers” could have devastating consequences if lab-grown reproductive cells were ever used in the clinic to assist reproduction. If even a single gene is wrongly imprinted by epigenetic marks, it could lead to serious disease.
Digging deeper, the team found an entire network of molecules that could explain why BMP2 triggered epigenetic reprogramming—even though it wasn’t complete. One possible reason is it altered the activity of a protein that adds epigenetic “tags” to DNA, “but further investigation will be necessary to determine the precise mechanism and whether this is direct or indirect,” said Saitou.
In vitro gametogenesis is still in its infancy, and there’s much left to learn. But with mice already born from lab-made eggs, there’s no doubt the field is rapidly advancing—along with weighty ethical and social questions. Lab-grown gametes offer a way to rapidly experiment with gene editing to cure diseases for the next generation. But like the notorious CRISPR babies, if fertilized, they could lead to permanently gene-edited humans with the capacity to pass genetic modifications along to their children.
Saitou is well aware of the risks, and he welcomes public discussion.
“Many challenges remain and the path will certainly be long, especially when considering the ethical, legal, and social implications associated with the clinical application of human IVG [in vitro gametogenesis],” he said. “Nevertheless, we have now made one significant leap forward towards the potential translation of IVG into reproductive medicine.”
Image Credit: Gerd Altmann / Pixabay
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles

In a First, Researchers Use Stem Cells and Surgery to Treat Spina Bifida in the Womb
These Supercharged Immune Cells Completely Eliminated Solid Tumors in Mice
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus
What we’re reading