mRNA Cancer Vaccines Spark Renewed Hope as Clinical Trials Gain Momentum

Share
When Angela received her first shot at the Lombardi Comprehensive Cancer Center in early 2020, Covid-19 was months away. Far from a household name, mRNA vaccines were mostly relegated to lab studies.
Yet the jab she received was made of the same technology. A melanoma patient, Angela had multiple malignant moles removed. Alongside an established immune-stimulating drug, the hope was the duo could fight off any residual cancerous cells and slash the chances of relapse.
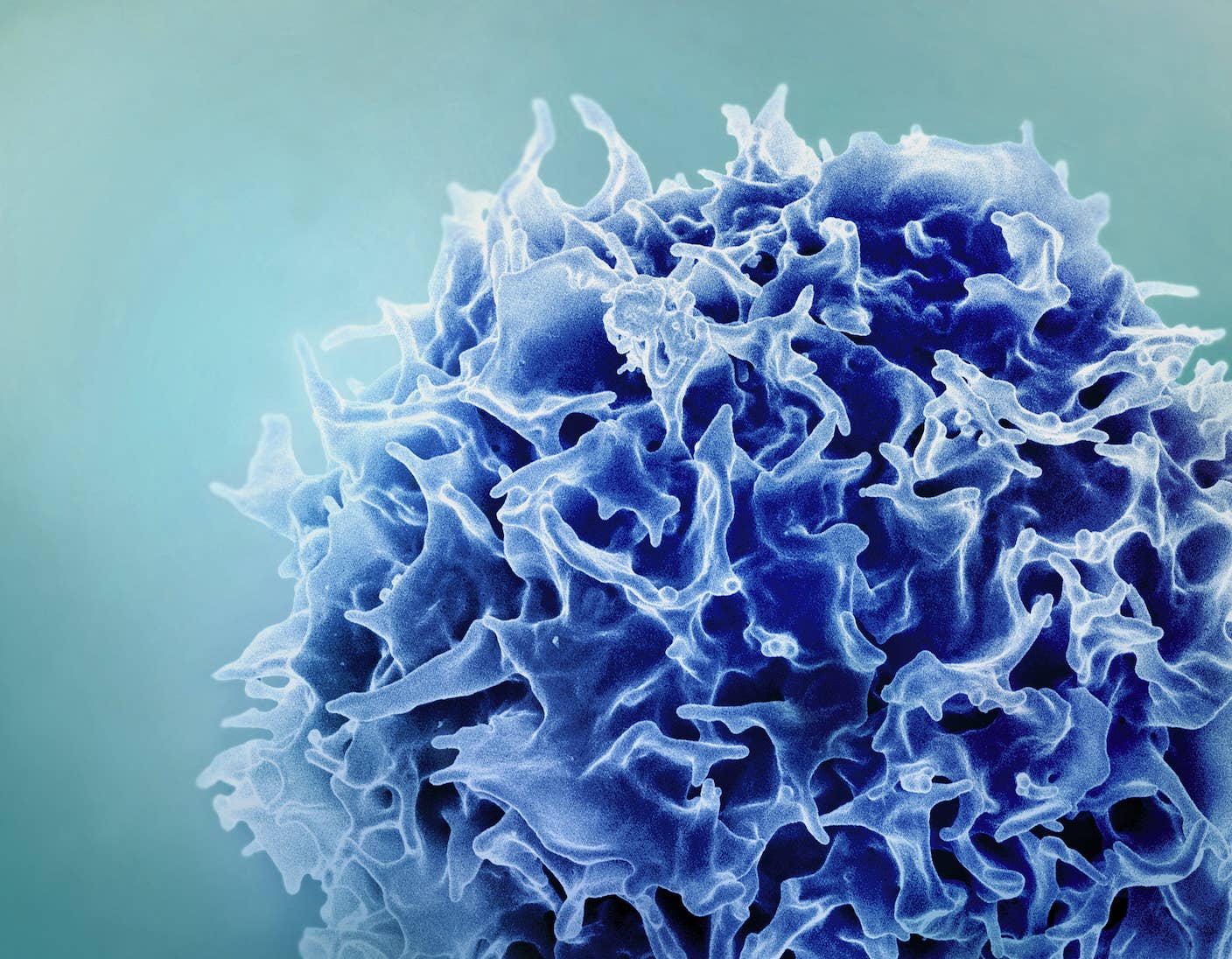
Scientists have long sought cancer vaccines that prevent the pesky cells from growing back. Like those targeting viruses, the vaccines would train the body’s immune system to recognize the cancerous cells and attack and eliminate them before they could grow and spread.
Despite decades of research into cancer vaccines, the dream has mostly failed. One reason is that every cancer, in every person, is different. So is each person’s immune system. Tailoring vaccines to neutralize cancers for each patient would not only be expensive, but sometimes impossible due to how long they’d take to develop—time is not on cancer patients’ sides.
In contrast, mRNA vaccines are far speedier to build. After they were removed, Angela’s malignant moles were analyzed for specific cancerous “fingerprints” or neoantigens. Based on these proteins, scientists at Moderna—known for their Covid-19 vaccines—built a custom mRNA cancer vaccine to train her immune system to prevent her own cancer from recurring.
Angela is part of clinical trial led by pharmaceutical companies Moderna and Merck to see if malignant skin cancer came back in patients given the treatment. Compared to a standard immunotherapy drug alone, adding a custom mRNA vaccine reduced the chances of cancer returning by roughly 50 percent and increased lifespan.
To be clear, the vaccines don’t protect a person from getting cancer in the first place. Rather, they teach the immune system to recognize residual malignant cells and prevent them from returning. The companies have launched Phase 3 clinical studies in people with melanoma and a type of lung cancer, with earlier stage clinical trials for other cancer cell types in the works.
Getting Personal
Like healthy cells, cancerous cells are dotted with all kinds of proteins on their surfaces. Dubbed “neoantigens,” these proteins differentiate cancer cells from healthy ones, making them attractive targets for therapies. And like fingerprints, neoantigens often differ between different cancer types and individuals, raising the possibility of personalized treatments.
That’s the idea behind cancer vaccines. They work like vaccines against infectious diseases. Parts of the invader—in cancer’s case, its unique neoantigens—are mixed with chemicals that stimulate the immune system. Once injected, the concoction directs the immune system to specifically attack cells with the neoantigen and eliminate the threat.
Compared to chemotherapy—notorious for its horrible side effects—cancer vaccines target a person’s own constellation of neoantigens, which in theory limits damage.
In 2017, two small clinical trials offered a glimpse that these vaccines could work in humans. Both studies targeted melanoma, a mole-like type of cancer that can quickly spread and recur.
After surgical removal, the researchers sequenced the genes of each malignant mole and selected up to 20 different protein fragments for each person to develop into vaccines. In one study, the shots kept the cancer at bay in four out of six patients for at least two years. The two who saw their cancer come back quickly entered remission after treatment with a drug that stimulates their immune system.
Another study enrolled 13 patients, eight with no visible tumors and five whose cancer had already spread. A personalized vaccine encoded 10 neoantigens for each person and used a virus to shuttle the mixture into cells. While successful for the first group, who remained cancer-free for over a year, results were mixed in the second group. For these patients, the cancer shrank but resurged in some, while others went into remission after treatment with the same immune-stimulating drug.
“It’s potentially a game changer,” Dr. Cornelis Melief at Leiden University Medical Center, who was not involved in the study, told Nature at the time.
Yet the field still faced a roadblock: Cancer vaccines are expensive to make and often require time—time that patients don’t always have.
An mRNA World
Enter mRNA vaccines. Best known for battling Covid-19, these vaccines can be designed and manufactured at a fraction of the time and cost of their traditional protein-based counterparts.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


A cancer vaccine based on mRNA follows a similar path to previous iterations, but with a few upgrades.
The patient’s skin cancer is rapidly sequenced for its genes after removal. Selection of neoantigen genes is key. Not all of them can be recognized by the immune system. Machine learning algorithms, trained on expanding databases of cancer-related mutations, sort through the data to identify the neoantigen genes most likely to stimulate the immune system. Moderna picks up to 34 candidates with the highest chances.
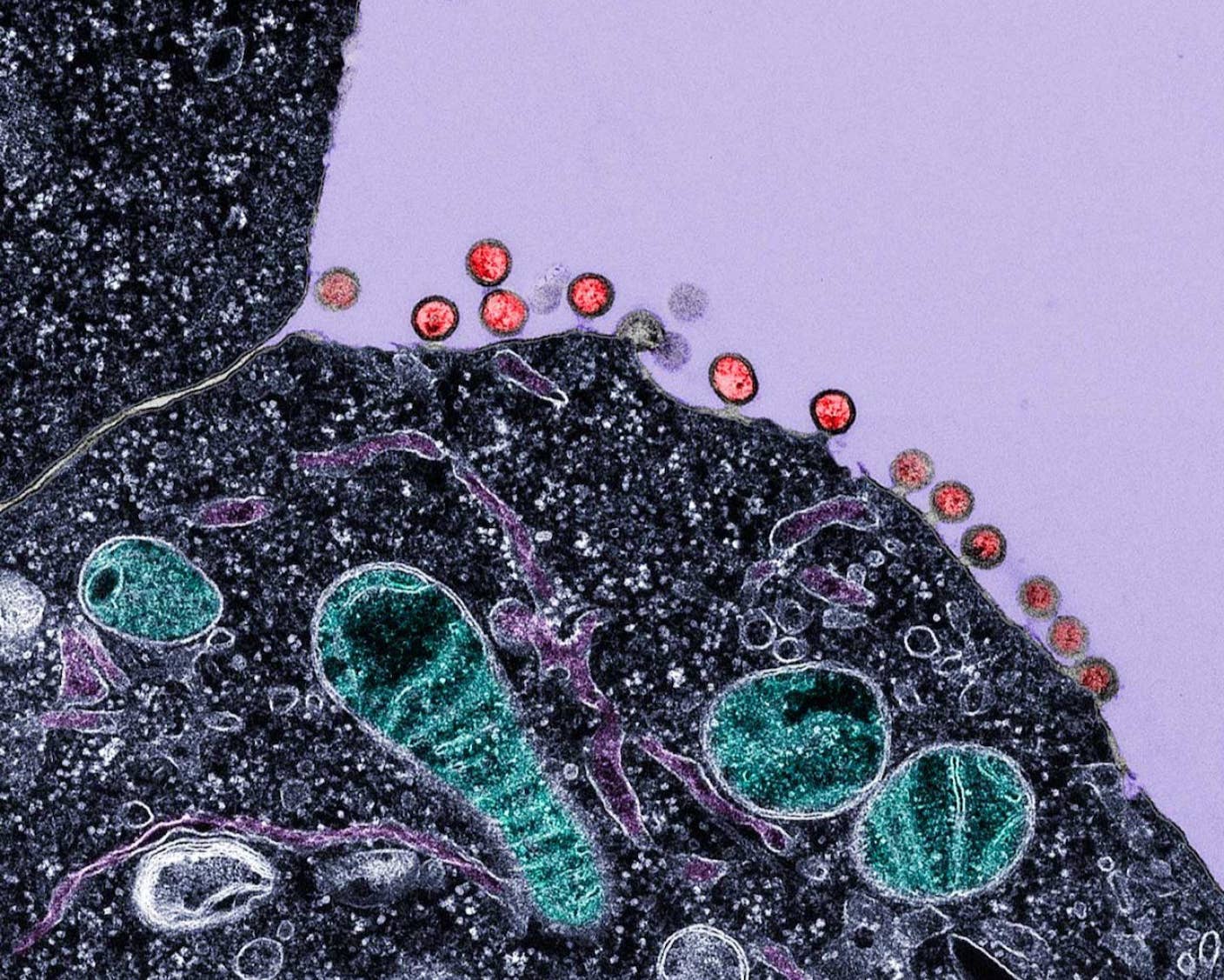
Like in Covid-19 vaccines, the selected genes are then translated into mRNA and encapsulated in fatty bubbles. Once injected, the mRNA commandeers the cell’s protein-making machinery to pump out neoantigens. These, in turn, train the immune system to sniff out the foe.
The mRNA vaccines weren’t used alone, however. Taking a note from previous studies, the companies added an immune-stimulating drug to boost efficacy.
The results from a three-year ongoing trial were announced earlier this month. The combination, compared to the drug alone, reduced the risk of cancers returning and death by 49 percent. They also decreased the risk of the cancer spreading by 62 percent. Living cancer-free for at least two and a half years, those treated with the combo saw a boost in their chances of survival with the addition of the mRNA vaccine. The results mirror those from a previous analysis, led by Dr. Jeffrey Weber at New York University Langone Health, who is overseeing the trial, dubbed KEYNOTE-942.
“At the end of the day, you realize, ‘Damn! This combination seems to have activity,’” Weber told Nature.
Although the results are promising, the combo isn’t for everyone. Later-stage cancers, especially those which have already spread, don’t respond well to the treatment. These tumors also rapidly grow—compared to their earlier counterparts—robbing scientists of precious time to develop the personalized vaccine.
Others are doing similar work. BioNTech has partnered with Genentech to develop vaccines targeting up to 20 neoantigens for notoriously aggressive pancreatic cancer. The vaccine worked for only half of the participants; even then, a fraction of the immune system only recognized one neoantigen. Nonetheless, vaccinated patients lived longer cancer-free after treatment when assessed 18 months after treatment.
Cancer vaccines are having a renaissance, but there’s much left to learn. Figuring out how to choose the right neoantigens is first and foremost. One team, for example, is verifying that immune cells in blood samples from patients actually recognize the selected neoantigens.
Other cancer types are already on the docket as potential next targets, including those that affect cells lining the skin, lungs, and digestive tracts, or those involved in kidney cancer.
As for Angela, the initial flu-like symptoms from the treatment were worth it. In her mid-40s, her cancer has been gone for three years. When asked if it’s because of the vaccine or drug, she told Nature: “I’m just happy to be cancer-free.”
Image Credit: Diana Polekhina / Unsplash
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
Single Injection Transforms the Immune System Into a Cancer-Killing Machine

New Gene Drive Stops the Spread of Malaria—Without Killing Any Mosquitoes
New Immune Treatment May Suppress HIV—No Daily Pills Required
What we’re reading