Latest Victory For Regenerative Medicine: Pituitary Grown From Embryonic Stem Cells

Share
Chalk up another part of the body that can be grown from stem cells – at least in mice. Scientists in Japan have induced mouse embryonic stem cells to form a pituitary in the lab. The team’s success not only holds promise for people with pituitary defects, but it’s another of just a few examples in which stem cells have been coaxed into a complex, three dimensional structure.
The pituitary is often referred to as the “master” gland of the endocrine system, as it secretes hormones that control the hormones secreted by other endocrine glands. It’s formation during embryonic development is closely tied to the hypothalamus, another important endocrine structure located close by at the base of the brain. The challenge to the Japanese researchers was to maintain the proper developmental environment for the nascent pituitary outside the brain. It was a complex challenge. They added hypothalamus tissue to the mix so that the stem cells would receive guiding signals from it, but the brain obviously consists of much more than these two areas. In order to “trick” the pituitary into thinking it was still in the brain, they also added several growth-inducing molecules including Sonic Hedgehog (it was discovered by a graduate student back when the game was popular) that are required for proper development in the brain. It worked. In just a couple weeks, the new structure not only looked like a pituitary, it produced all the major molecular markers that a normal pituitary produces. For the icing on the cake, the researchers placed the lab-grown pituitary into mice which had their own pituitaries destroyed. A week after transplantation, the mice showed increased blood levels of hormones produced by the pituitary.
The study was led by Yoshiki Sasai at the Riken Institute in Japan and was published in Nature.
The pituitary hormones regulate important physiological processes such as growth, puberty, and reproduction. A dysfunctional pituitary can lead to deficits in these hormones, which in turn can lead to disorders such as stunted growth, hypothyroidism, and infertility. Combined pituitary hormone deficiency affects about 1 in 3,000 to 4,000 live births. And although hormone-replacement therapy can be effective for many, it does not return hormone levels to their normal levels.
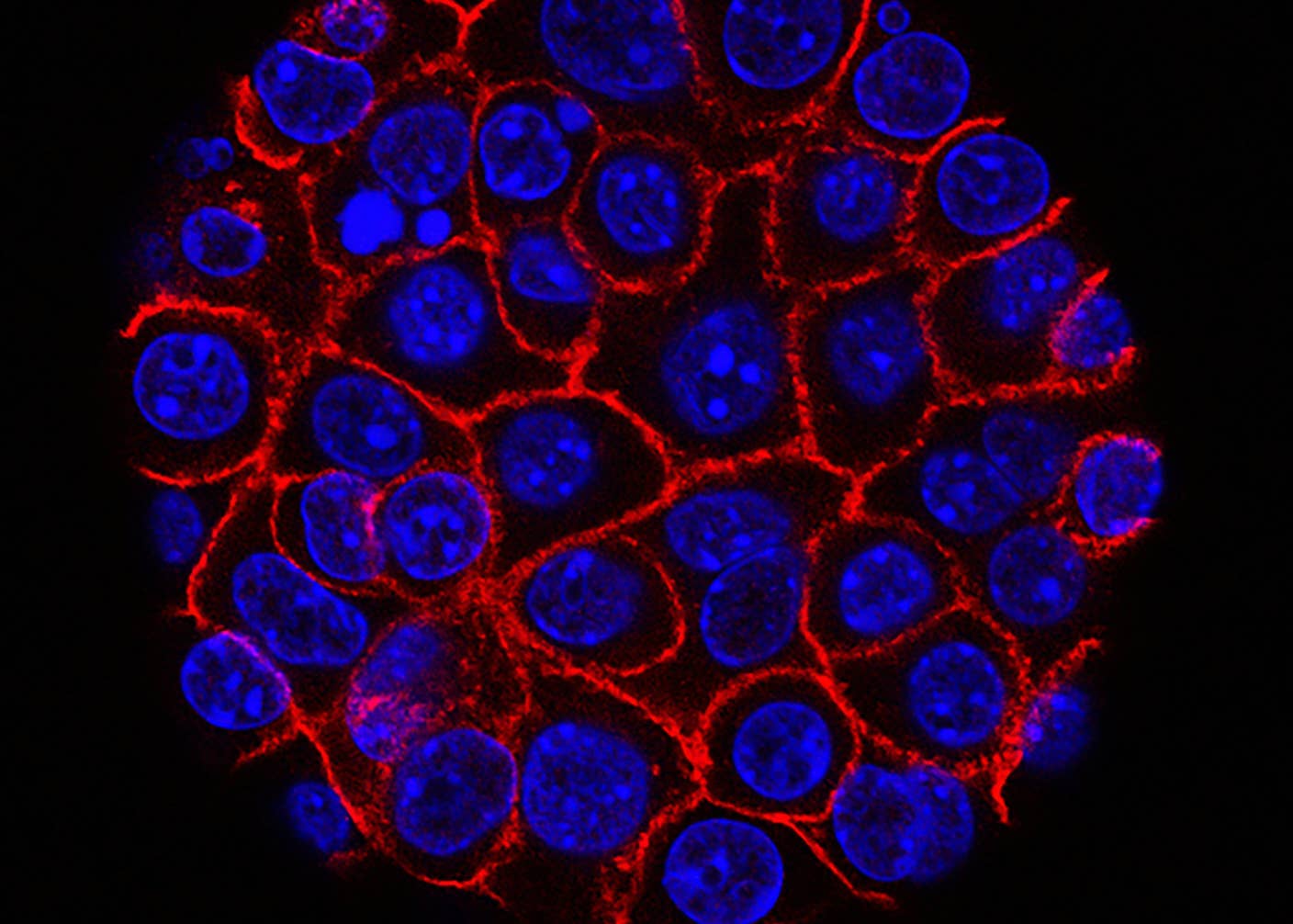
But don’t expect doctors to start replacing dysfunctional pituitaries with ones grown in the lab anytime soon. Most importantly, we’ll first need to see if the procedure can be repeated with human embryonic stem cells. And even now questions remain regarding the lab-grown mouse pituitaries. Embryonic stem cells differentiated in the lab don’t always run the course to full maturity. The pituitary in the current study still looks like the pituitary from an embryo. Only time will tell whether or not it can develop to an adult pituitary. But even if we can’t start swapping out dysfunctional pituitaries, the lab-grown structures should be a valuable tool for researchers studying pituitary defects. They can be looked at under a microscope and labeled with molecular markers, lending themselves to analyses far more difficult to perform in whole animals.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


It could also pave the way for future stem cell research. The pituitary’s development in the study, as it is in normal development, was dependent on molecular signals sent from the hypothalamus. Now that the researchers have established that it is possible to run this inductive process, they have opened the door for the induction of even more complex organs in the lab.
The victories for regenerative medicine just keep on coming. Last year a group at UC Irvine in California successfully grew a retina from human embryonic stem cells. Like the pituitary, the retina needed to be grown with a specific three-dimensional organization in order to function properly. The starting clumps of stem cells required no intervention from the scientists to become retinas. The cell-to-cell communication during “development” was all they needed. Sasai’s group also induced embryonic stem cells to form a retina this past spring, although theirs was grown from mouse cells.
The group is currently working to improve transplantation of pituitary tissue in their mouse model. They're also working on methods to repeat the experiment with human stem cells. Sasai expects it will be about three years to create a human pituitary. When they do, the field of regenerative medicine will be that much closer to its holy grail of growing all organs in the lab and transplanting them into humans.
Peter Murray was born in Boston in 1973. He earned a PhD in neuroscience at the University of Maryland, Baltimore studying gene expression in the neocortex. Following his dissertation work he spent three years as a post-doctoral fellow at the same university studying brain mechanisms of pain and motor control. He completed a collection of short stories in 2010 and has been writing for Singularity Hub since March 2011.
Related Articles
These Supercharged Immune Cells Completely Eliminated Solid Tumors in Mice

New Device Detects Brain Waves in Mini Brains Mimicking Early Human Development

This Week’s Awesome Tech Stories From Around the Web (Through February 28)
What we’re reading

