Largest Genetic Study to Date Unveils DNA Profiles That Lead to Cancer

Share
Cancers are like malicious snowflakes. Each harbors a unique set of mutations in its genes, gradually turning them to the dark side. Eventually, with no regard for their neighbors, mutated cells destroy tissues, organs, and life.
But their set of genetic mutations—a signature—can also be their downfall. Like fingerprints or DNA left at a crime scene, we can use those signatures to hunt down cancerous cells, nailing the culprits with medication while leaving innocent, healthy cells alone.
The key is a database documenting these signatures. Fingerprints are useless if there’s nothing to match them against. Family-tree sleuthing wouldn’t be possible without open-sourced genealogy sites. Similarly, to chase down biological terrorists like cancer, we need a whole ledger of genetic mutation culprits as a reference.
We just got it. In a massive study covering over 12,000 tumors, a team from the UK mapped out genetic changes that lead normal cells to develop into cancerous ones. A treasure trove, the dataset captured unique genetic “fingerprints” of common types of cancer, but also rare individual mutations that reflect a person’s history.
The study and its resulting catalog is the largest of its kind. Comparing the new mutation atlas to previous studies, the team found 58 new ones, which clued them in to potential genetic changes and lifestyle factors that drive cancer. They next developed an algorithm to match up mutational signatures in the database to new tissue samples, building a whole crime scene investigation system for cancer screening.
“The reason it is important to identify mutational signatures is because they are like fingerprints at a crime scene—they help to pinpoint cancer culprits,” said the study’s lead author, Dr. Serena Nik-Zainal at the University of Cambridge. “Some mutational signatures have clinical or treatment implications—they can highlight abnormalities that may be targeted with specific drugs or may indicate a potential ‘Achilles heel’ in individual cancers.”
The Turning
We have roughly 30 billion cells in our bodies. With age, each cell’s genome slowly changes its DNA letters.
"Right now every cell in my body is accumulating mutations, so if they live long enough it will be inevitable that they will end up developing a tumor," said Nik-Zainal. "Having said that, let's remember that a human is made of 30 billion cells, all accumulating mutations, and only one of them will start a cancer throughout my life. This is amazing.”
So why do some normal cells go bad?
We’ve known for decades that copy edits to DNA can flip oncogenic—or pro-cancer genes—on, while shutting off genes that normally protect against this process. Cancer cells also divide more often than normal cells. These discoveries led to powerful treatments, including chemotherapy and immunotherapies.
But these insights are relatively crude, like painting the genomic landscape of cancer with a wide brush stroke; little individuality seeps in. And with cancer, the uniqueness of both the host and the pattern of genetic mutations matter.
Enter mutational signatures.
Here, the focus is on changes in the precise lettering of DNA as a cell turns cancerous. Different cancer types have distinct mutations while sharing certain commonalities. These signatures capture both the habits of the host—for example, if they smoke—and the cancer itself, such as being unable to repair damaged DNA.
In other words, a mutational signature captures a specific pattern of DNA letter changes and repairs into a highly personalized fingerprint of a person’s cancer. As with actual fingerprints, there are similarities between different people and cancers. The study took a clever route: first, they hunted down common signatures in cancers from different organs and people. They then cross-examined signatures between organs, eventually nailing down 120 key mutational signatures common across all the study’s cancers.
The process is like taking photos of different faces, but eventually blending them together to find commonalities in features, while also highlighting differences.
The team lucked out with a massive asset: the 100,000 Genomes Project of Genomics England, which sequenced the whole genome of tens of thousands of people. It “has a greater number of whole-genome sequences than previous major cancer sequencing projects put together,” said Dr. Dávid Szüts at the Research Center for Natural Sciences in Budapest, who was not involved in the study. “Because the mechanism behind many signatures is still unknown, the study…also provides fertile ground for further investigation.”
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


A Rainbow of Mutations
All together, the team screened for single or double DNA letter changes in 12,222 cancer samples. The resulting dataset was a beast to slay. To fish out mutational signatures, they developed a computational method that parses common mutations from rarer ones. As a sanity check, the team validated their findings by matching up their data from two open-sourced databases, each containing roughly 3,000 cancer samples.
[We looked at] “thousands and thousands of mutations, and that gives us a lot of power to be able to look at patterns across patient samples,” said Nik-Zainal.
For each organ, the team found just 5 to 10 common signatures, suggesting a common thread in cancers that could be co-opted for better treatment. Matching signatures across organs, they found 58 new fingerprints, which were compared to a previous global attempt at documenting cancer mutations. Some were common across patients; others more unique, teasing out the “snowflake” character of cancers.
With further detective work, they hunted down potential causes for the mutation signatures. Some culprits were already well known: nip-tucks that compromise the DNA’s ability to repair itself after a break.
Others revealed more enigmatic damage. One signature for brain tumors, for example, was surprisingly similar to samples blasted with UV light. Exposure to platinum matched up with multiple types of cancers, including ovary, stomach, and breast cancer. Another signature, dubbed SBS4 (yeah, they don’t have the catchiest names) is highly associated with tobacco use, but with a surprising match to breast and colon cancer—potentially, a target for drug development to kill multiple birds with one stone.
Similar to colors, mutational signatures can be combined into a spectra—a rainbow of different mutation profiles. If that sounds complex, it’s because cancer is extremely complex. Different signatures can help us deconstruct a complex, cancerous genetic recipe so we can understand it and in turn know how to control it.
What Next?
Fingerprinting cancer genomes isn’t exactly eye-catching, but the database could propel the next generation of cancer treatments.
The amount of information is staggering—even the authors admitted to throwing up their hands at further analyses. Instead, they developed and released an algorithm that fits new cancer genetic data to the dataset. Dubbed FitMS, or Signature Fit Multi-Step, the software takes the same approach as the study: fitting signatures to common ones first, then broadening the scope to identify additional rare signatures.
The tool is freely available so that doctors can match up a new tissue sample to the database. This “signature-fitting” process can, in theory, diagnose and tailor the patient’s cancer treatment to their particular set of mutations.
“This study shows how powerful whole genome sequencing tests can be in giving clues into how the cancer may have developed, how it will behave, and what treatment options would work best,” said Michelle Mitchell from Cancer Research UK.
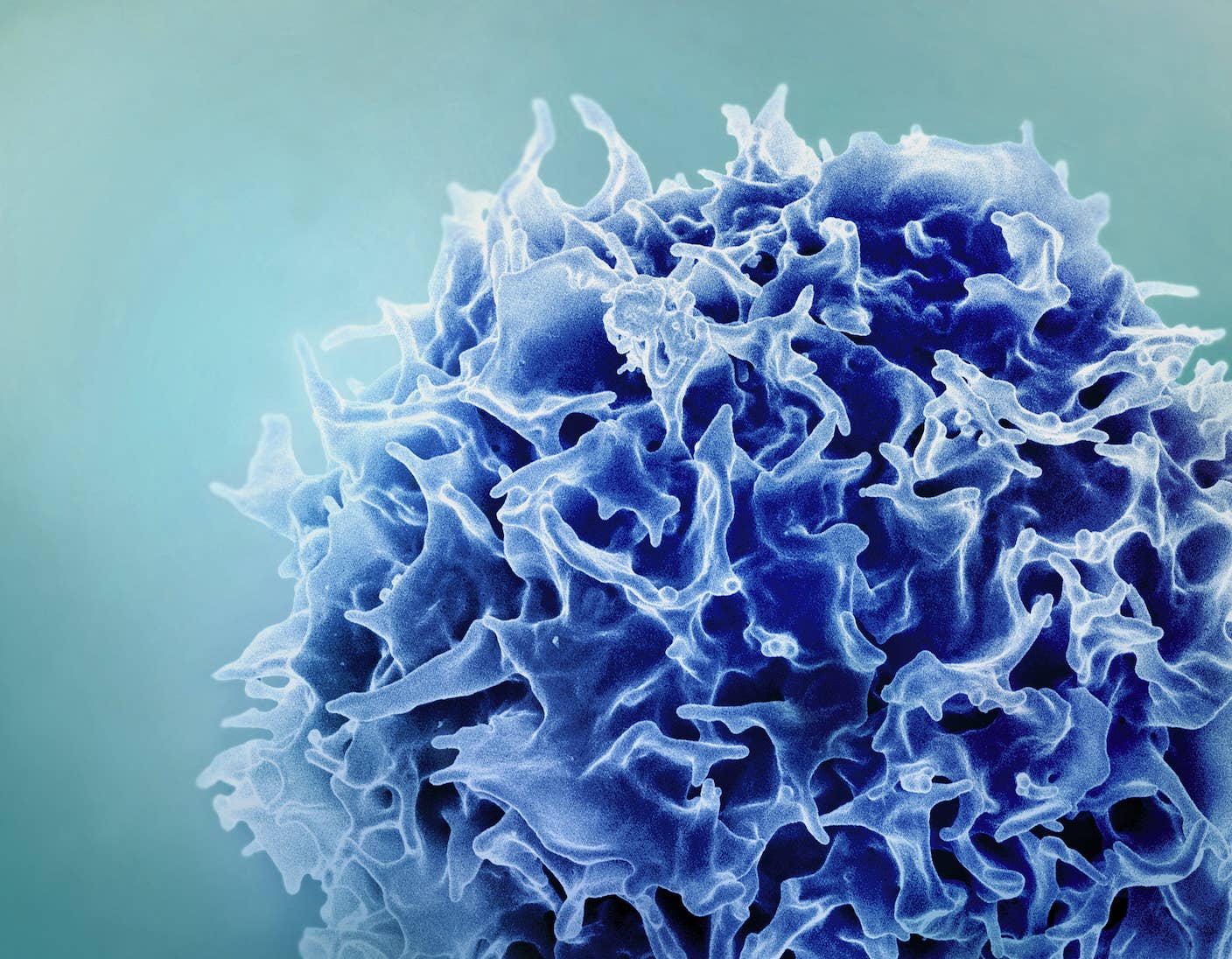
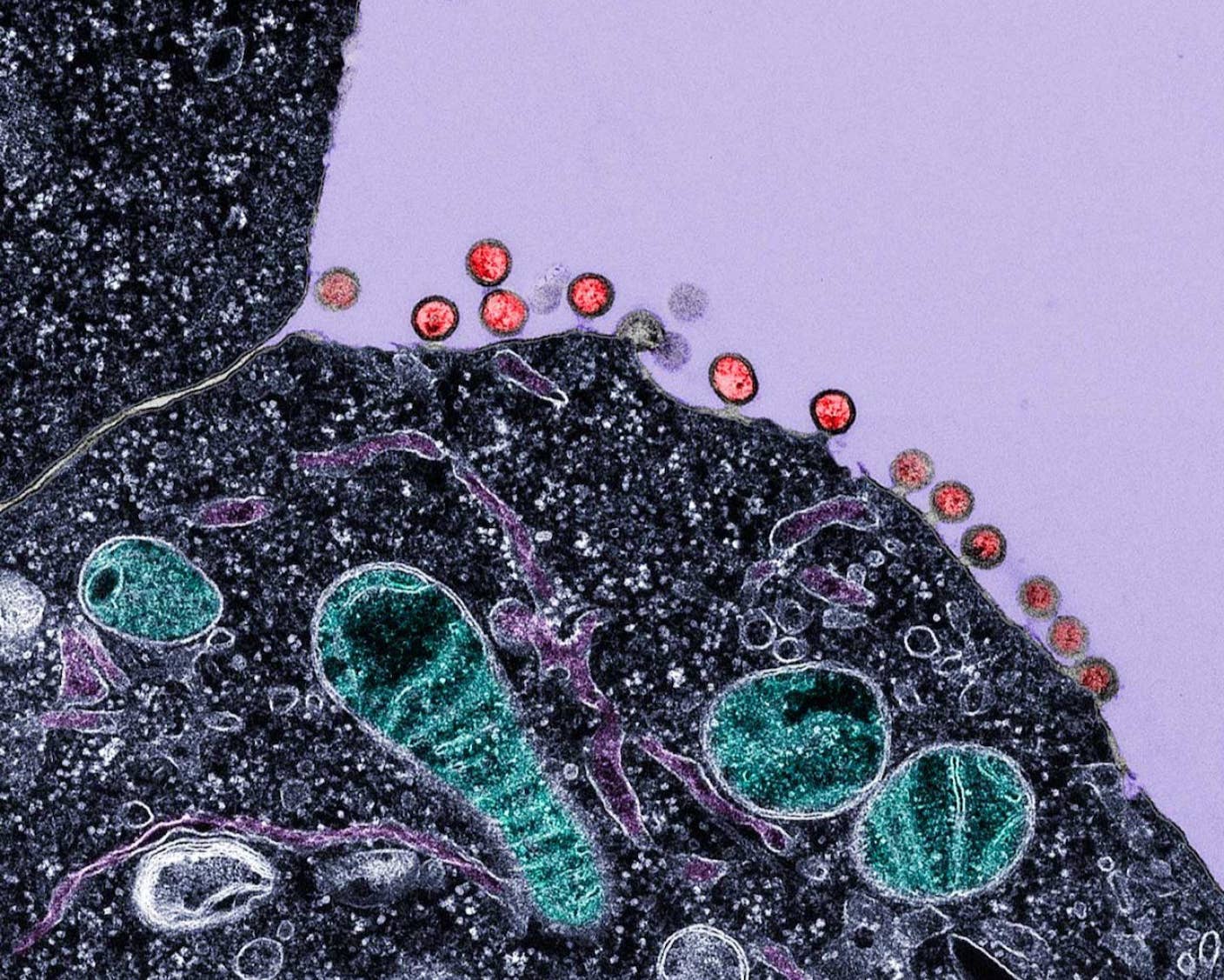
Image Credit: Zita / Shutterstock.com
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
Single Injection Transforms the Immune System Into a Cancer-Killing Machine

New Gene Drive Stops the Spread of Malaria—Without Killing Any Mosquitoes
New Immune Treatment May Suppress HIV—No Daily Pills Required
What we’re reading