Cell Therapies Now Beat Back Once Untreatable Blood Cancers. Scientists Are Making Them Even Deadlier.
Share
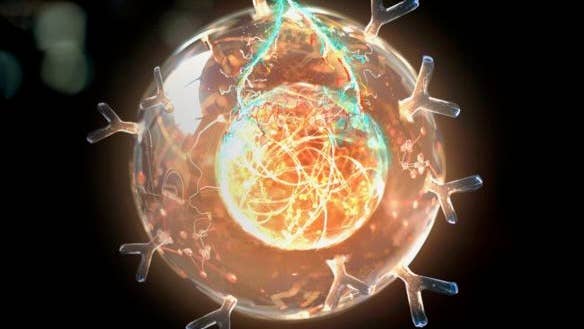
Dubbed “living drugs,” CAR T cells are bioengineered from a patient’s own immune cells to make them better able to hunt and destroy cancer.
The treatment is successfully tackling previously untreatable blood cancers. Six therapies are already approved by the FDA. Over a thousand clinical trials are underway. These aren’t limited to cancer—they cover a range of difficult medical problems such as autoimmune diseases, heart conditions, and viral infections including HIV. They may even slow down the biological processes that contribute to aging.
But CAR T has an Achilles heel.
Once injected into the body, the cells often slowly dwindle. Called “exhaustion,” this process erodes therapeutic effect over time and has dire medical consequences. According to Dr. Evan Weber at the University of Pennsylvania, more than 50 percent of people who respond to CAR T therapies eventually relapse. This may also be why CAR T cells have struggled to fight off solid tumors in breast, pancreatic, or deadly brain cancers.
This month, two teams found a potential solution—make CAR T cells more like stem cells. Known for their regenerative abilities, stem cells easily repopulate the body. Both teams identified the same protein “master switch” to make engineered cells resemble stem cells.
One study, led by Weber, found that adding the protein, called FOXO1, revved up metabolism and health in CAR T cells in mice. Another study from a team at the Peter MacCallum Cancer Center in Australia found FOXO1-boosted cells appeared genetically similar to immune stem cells and were better able to fend off solid tumors.
While still early, “these findings may help improve the design of CAR T cell therapies and potentially benefit a wider range of patients,” said Weber in a press release.
I Remember
Here’s how CAR T cell therapy usually works.
The approach focuses on T cells, a particular type of immune cell that naturally hunts downs and eliminates infections and cancers inside the body. Enemy cells are dotted with a specific set of proteins, a kind of cellular fingerprint, that T cells recognize and latch onto.
Tumors also have a unique signature. But they can be sneaky, with some eventually developing ways to evade immune surveillance. In solid cancers, for example, they can pump out chemicals that fight off immune cell defenders, allowing the cancer to grow and spread.
CAR T cells are designed to override these barriers.
To make them, medical practitioners remove T cells from the body and genetically engineer them to produce tailormade protein hooks targeting a particular protein on tumor cells. The supercharged T cells are then grown in petri dishes and transfused back into the body.
In the beginning, CAR T was a last-resort blood cancer treatment, but now it’s a first-line therapy. Keeping the engineered cells around inside the body, however, has been a struggle. With time, the cells stop dividing and become dysfunctional, potentially allowing the cancer to relapse.
The Translator
To tackle cell exhaustion, Weber’s team found inspiration in the body itself.
Our immune system has a cellular ledger tracking previous infections. The cells making up this ledger are called memory T cells. They’re a formidable military reserve, a portion of which resemble stem cells. When the immune system detects an invader it’s seen before—a virus, bacteria, or cancer cell—these reserve cells rapidly proliferate to fend off the attack.
CAR T cells don’t usually have this ability. Inside multiple cancers, they eventually die off—allowing cancers to return. Why?
In 2012, Dr. Crystal Mackall at Stanford University found several changes in gene expression that lead to CAR T cell exhaustion. In the new study, together with Weber, the team discovered a protein, FOXO1, that could lengthen CAR T’s effects.
In one test, a drug that inhibited FOXO1 caused CAR T cells to rapidly fail and eventually die in petri dishes. Erasing genes encoding FOXO1 also hindered the cells and increased signs of CAR T exhaustion. When infused into mice with leukemia, CAR T cells without FOXO1 couldn’t treat the cancer. By contrast, increasing levels of FOXO1 helped the cells readily fight it off.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Analyzing genes related to FOXO1, the team found they were mostly connected to immune cell memory. It’s likely that adding the gene encoding FOXO1 to CAR T cells promotes a stable memory for the cells, so they can easily recognize potential harm—be it cancer or pathogen—long after the initial infection.
When treating mice with leukemia, a single dose of the FOXO1-enhanced cells decreased cancer growth and increased survival up to five-fold compared to standard CAR T therapy. The enhanced treatment also tackled a type of bone cancer in mice, which is often hard to treat without surgery and chemotherapy.
An Immune Link
Meanwhile, the Australian team also zeroed in on FOXO1. Led by Drs. Junyun Lai, Paul Beavis, and Phillip Darcy, the team was looking for protein candidates to enhance CAR T longevity.
The idea was, like their natural counterparts, engineered CAR T cells also need a healthy metabolism to thrive and divide.
They started by analyzing a protein previously shown to enhance CAR T metabolism, potentially lowering the chances of exhaustion. Mapping the epigenome and transcriptome in CAR T cells—both of which tell us how genes are expressed—they also discovered FOXO1 regulating CAR T cell longevity.
As a proof of concept, the team induced exhaustion in the engineered cells by increasingly restricting their ability to divide.
In mice with cancer, cells supercharged with FOXO1 lasted longer by months than those that hadn’t been boosted. The critters’ liver and kidney functions remained normal, and they didn’t lose weight during the treatment, a marker of overall health. The FOXO1 boost also changed how genes were expressed in the cells—they looked younger, as if in a stem cell-like state.
The new recipe also worked in T cells donated by six people with cancer who had undergone standard CAR T therapy. Adding a dose of FOXO1 to these cells increased their metabolism.
Multiple CAR T clinical trials are ongoing. But “the effects of such cells are transient and do not provide long-term protection against exhaustion,” wrote Darcy and team. In other words, durability is key for CAR T cells to live up to their full potential.
A FOXO1 boost offers a way—although it may not be the only way.
“By studying factors that drive memory in T cells, like FOXO1, we can enhance our understanding of why CAR T cells persist and work more effectively in some patients compared to others,” said Weber.
Image Credit: Gerardo Sotillo, Stanford Medicine
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles

Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading