A One-Shot Remedy for Asthma? New Study in Mice Paves the Way
Share
Imagine trying to breathe through a plastic bag. You struggle. Your heart starts to race. Your head gets dizzy. And all you did was stroll through a park full of blooming flowers.
Asthma is one of the most common breathing disorders in the world, affecting over 300 million people. Inhalers can temporarily open airways in emergencies, but there’s no cure.
Now, scientists from Tsinghua University in Beijing have found a way to keep asthma attacks in check with just a single shot. Using CAR T cell therapy, they designed a “living drug” to hunt down one of the main triggers for asthma, a group of immune cells called eosinophils. The treatment reduced lung inflammation and warded off asthma symptoms in mice for six months. In multiple asthma models, the therapy lowered lung inflammation, quieted eosinophils in the airways, and re-opened airways.
Managing asthma currently focuses on relieving symptoms and requires nearly life-long treatment. The study suggests a single CAR T dose could keep asthma at bay, “marking a potential paradigm shift in the management of common chronic disease,” the team wrote in a paper published in Nature Immunology.
Chronic Dilemma
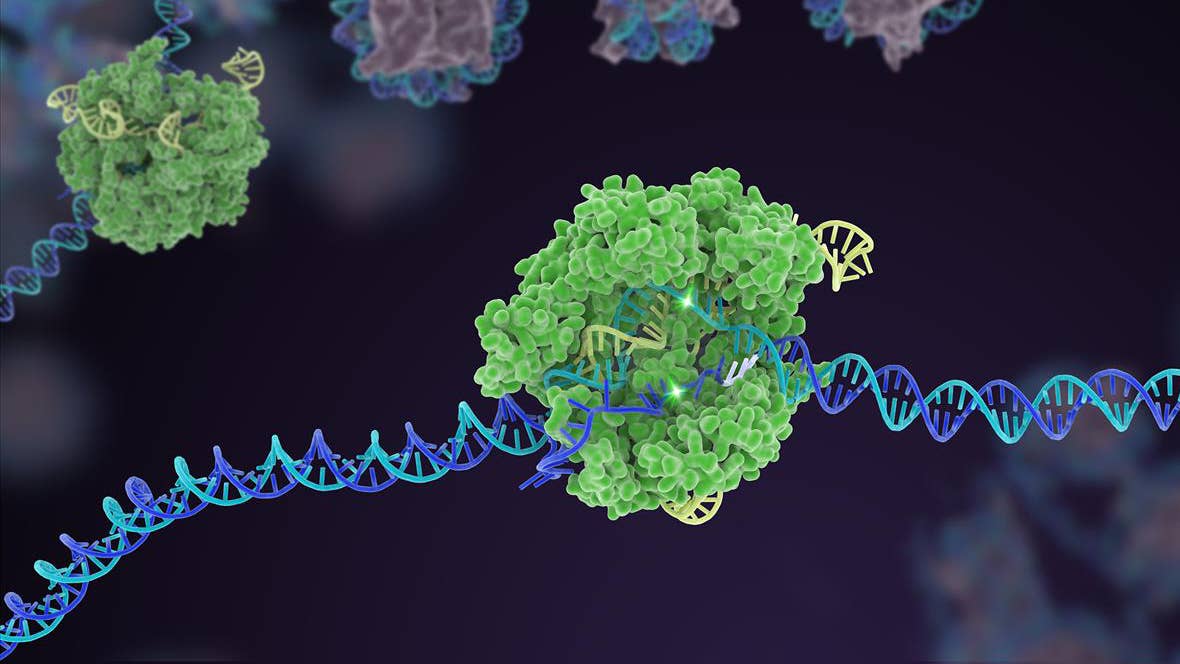
In CAR T cell therapy, scientists extract T cells from the body, genetically engineer them to produce protein “hooks” that grab onto a target of interest—say, a cancer cell—and infuse them back into the body. The amped-up cells then hunt down and destroy the enemy.
This protein handshake is the core of CAR T. Proteins dotted along the surfaces of T cells—a type of immune cell—readily grab onto another protein target. Targets can be on the surfaces of other cells, bacteria, or even viruses, such as HIV. Thanks to CRISPR-Cas9 and other gene editing tools, adding customized protein “hooks” is easier and more efficient than ever.
Six CAR T therapies have been approved for a variety of blood cancers. Meanwhile, scientists are exploring whether CAR T can tackle glioblastoma—an especially difficult type of brain cancer—autoimmune disorders, Type 1 diabetes, or even aging.
But CAR T therapy for chronic disorders is still difficult, the authors wrote in the paper.
The first challenge is finding the right target. In blood cancer, the revamped T cells are like molecular torpedoes that mercilessly seek and destroy tumor cells. But chronic illnesses often involve a myriad of cells and proteins working together, and they can affect multiple organs. This makes finding a target more difficult, especially if the target has some normal uses too.
The second is longevity. CAR T cells divide like other cells, but over time some get worn out and no longer renew. These exhausted T cells eventually die off, and the disease rebounds.
Then there’s the potential of an immune civil war. For blood cancers, people need to undergo chemotherapeutic conditioning of the bone marrow—a source of immune cells—to make space for the new modified cells. It’s a necessary step, and though grueling, is acceptable for devasting diseases. But serious side effects make it a tough call for non-life-threatening diseases.
The new study took in all these concerns and engineered a single shot CAR T solution for asthma without the need for conditioning.
Long Live CAR T
In asthma, eosinophils infiltrate the airways.
These white blood cells usually fight off infection. But when overzealous, they trigger hyper-inflammation and damage delicate cells lining the lungs. Mucus also builds up and blocks the airways. Meanwhile, a soup of immune molecules accumulates and adds to the inflammation.
Drugs targeting immune molecules have been approved for asthma, but they only provide temporary relief, wrote the authors. They don’t cure the disorder, and because they need to be taken constantly over years or even decades, they’re not cost effective.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


The new study sought to lower eosinophil levels by targeting IL-5R, a protein on the cells’ surfaces. It’s not the first time scientists have tried the strategy. A previous study that inhibited IL-5R function using antibodies was found to be safe in patients, but it required repeated dosing and risked the body becoming immune to the antibodies.
The team genetically added protein “hooks” targeting IL-5R onto T cells extracted from mice and transferred a million of the CART cells back into the mice without any conditioning. Surprisingly, the experiment was a dud. The cells died off in a week, and eosinophil levels bounced back.
What now? Earlier this year, the same team found that wiping away two genes transformed T cells into an “immortal-like” state. In a second try, they added the IL-5R-targeting protein to these T cells. It worked. When infused into mice, the upgraded cells expanded and flourished, and they lived happily alongside unmodified T cells in tissues in the lung and liver.
In multiple types of asthma models, the CAR T cells damped lung inflammation and dramatically lowered eosinophil levels. When given four weeks before an especially severe asthma attack induced by chemicals, the therapy protected against lung inflammation and symptoms.
For a more “real-life” scenario, the team next turned to dust mites—a common trigger for asthma and allergy attacks. They exposed mice to dust mites for roughly two months (a bit like living in a dusty basement) and then gave them a shot of CAR T cells or an antibody treatment previously used to reduce asthma symptoms. Four weeks later, the CAR T cell treatment was more effective at reducing mucus buildup and keeping lung inflammation at bay.
But would the therapy last? The team followed severely asthmatic mice for six months after the CAR T shot. The engineered cells lowered lung inflammation and kept the mice chipper and healthy—even when challenged with another asthma trigger.
Immune complications were a worry. But the treatment proved safe. The mice had normal bone marrow and spleen function—both sites generate blood and immune cells. During an asthma attack, CAR T cells rapidly expanded in numbers to lower eosinophil activity. With the job done, they fell back to a baseline “surveillance” number, without stressing the body.
Compared to natural T cells, the genetically altered “immortal-like” cells are perfect for long-lasting CAR T therapies, wrote the authors. In other tests, they added a mechanism into the cells to block an inflammatory protein in addition to eosinophils, with even better results.
The study is the latest example of CAR T therapy beyond cancer. But there’s still reason to be careful. In cancer treatments, the Food and Drug Administration (FDA) is investigating the risk of developing secondary tumors. This likely depends on the protein target, but long-living CAR T cells could also have unforeseen side effects, especially if used for chronic diseases.
For now, the team is planning to test a similar strategy in allergies and other breathing diseases related to eosinophils, such as chronic obstructive pulmonary disease (COPD).
Image Credit: crystal light / Shutterstock.com
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading