Biological Microchip Mimics a Real Lung – It Even Breathes!
Share
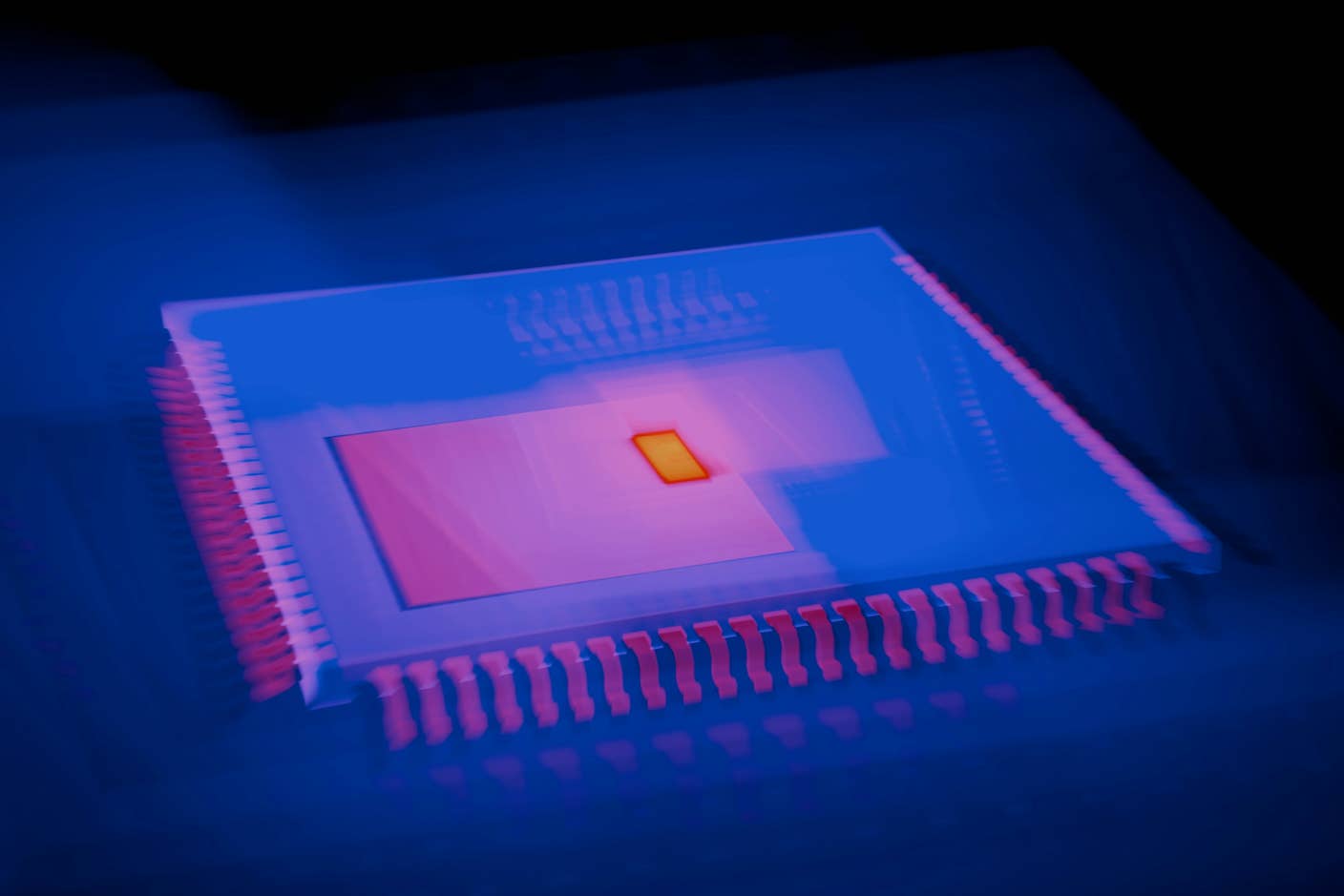
Who says biology, engineering, and medicine are different fields? Researchers led by Dr. Donald Ingber at Harvard’s Wyss Institute reported in Science that they have engineered a coin-sized microchip that can be loaded with wet biological cells, mimicking the workings of an actual lung. The bioinspired chip can be used to model drug action, determine the effects of environmental toxins, and could even replace some animal testing – all while speeding up research and dropping its costs.
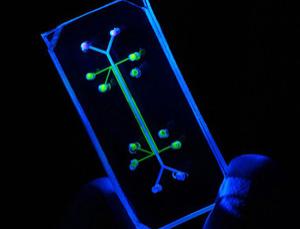
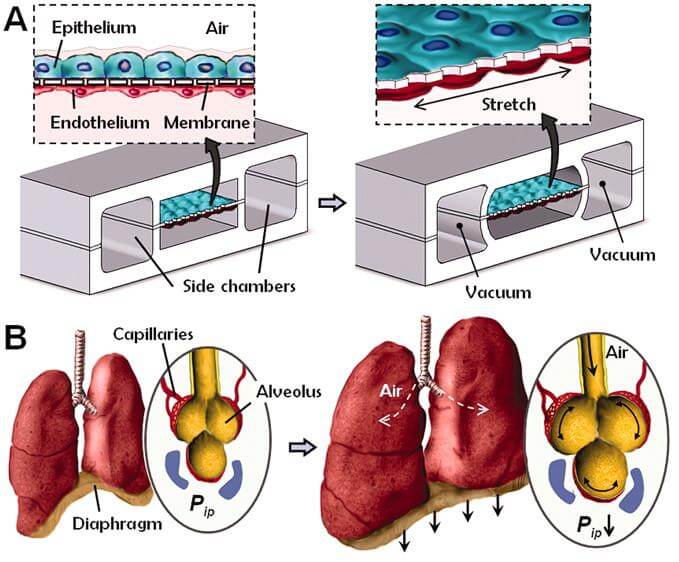
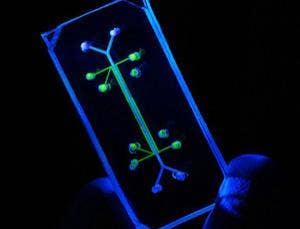
To mimic the physiology of an actual lung, the chip contains two chambers separated by a flexible, porous membrane. One chamber contains human lung cells (alveoli), which are tiny air sacs with thin walls – this chamber allows researchers to introduce foreign particles, just as breathing would do in an organism. Across the membrane, the second chamber contains capillary blood cells (endothelium) which normally take up particles into the blood stream, as well as interface the immune system with potential toxins and pathogens. The computer chip is transparent, which allows real-time observation of how the cells respond to introduced particles.
Did I mention it also breathes? Because the chip is flexible, fluctuating the air pressure within a network of channels along its surface can replicate the mechanics of breathing – stretching and expanding the cells inside the chambers, roughly as they would in real life. This capacity for the chip to mimic breathing is an important step forward, because cell culture techniques are unable to replicate how mechanical factors influence cell behavior. Filling this gap brings laboratory models closer to the real-world organs they try to represent. Think of it as a miniature version of the donated lungs made to breathe outside the body. Check out this video of lead researcher Donald Ingber talking about the chip:
Researchers’ first test of the lung-chip looked at how the system responded to the introduction of a pathogen. E. coli was added to the first chamber containing lung cells, mimicking the exposure of lungs to airborne bacteria. The second chamber was given a healthy dose of white blood cells (leukocytes), which are the immune system’s first line of defense against foreign invaders. Show time. Through the transparent chip, researchers watched in real time as the white blood cells migrated across the porous membrane, engulfing and killing the bacterial invaders. The chip clearly modeled the body’s own inflammatory response to pathogens.
A second test looked at how the lung-chip responded to the introduction of nanoparticles comparable to those found in toxic pollutants. Some of the particles induced an immune response and were trapped; others crossed the chip’s membrane and entered the blood chamber. Using the chip to model the introduction of non-biological particles illustrates how some toxins can make their way past the immune system and invade the body. It also provides an excellent system to test how airborne drugs are taken up into the lungs, which will cut costs and save time in the development of inhaled medications.
The next step? Currently, the cells used come from immortalized cell lines, which aren’t patient-specific and only provide a kind of average response to different drugs. If the lung-chip could be loaded with “primary” cells from an individual patient, testing could determine individual responses to potential drug action. Induced pluripotent stem cells, which can be derived from a patient’s skin, could be stimulated into alveoli and endothelium cells and provide a personalized lung-chip for specific testing. This would fit well into the larger movement towards patient-specific medicine.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


The lung-chip isn’t quite ready for broad application yet – it still needs to be cross-compared with current methods of testing inhalant effects, which use rats as experimental organisms. If these comparisons show that the chip accurately mimics a normal lung, it could eventually mean an end to animal testing for this type of research. In addition to the obvious win for animal rights folks, the chip would save time and money by replacing costly animal research.
Future research will plan to apply comparable techniques to other organs of the body – a gut-chip, kidney-chip, heart-chip, etc. This will help us understand how drugs and toxins effect the body more broadly. Imagine having a series of personalized chips for all your different organs – your doctors could custom-test any potential treatment against miniature models of your own body. The computer/body interface is already being explored with chips that can detect cancer or identify bacterial strains within the body; the lung-chip represents an exciting new application of this hybrid technology outside the body.
It's worth recognizing how exciting the Wyss Institute itself is. Founded last year by Ingber himself, the institute is devoted to biologically-inspired engineering: figuring out mother nature's tricks, and replicating them in man-made systems. The faculty list reads like a who's-who of biology (George Church and James Collins, to name a few) and if this research is any indication, we can expect more exciting research from this group in the future.
As it stands, the lung-chip is an amazing example of how biology is creating new frontiers in engineering: an impressive reminder of the sort of human-machine interface that represents the future of medicine, and potentially ourselves.
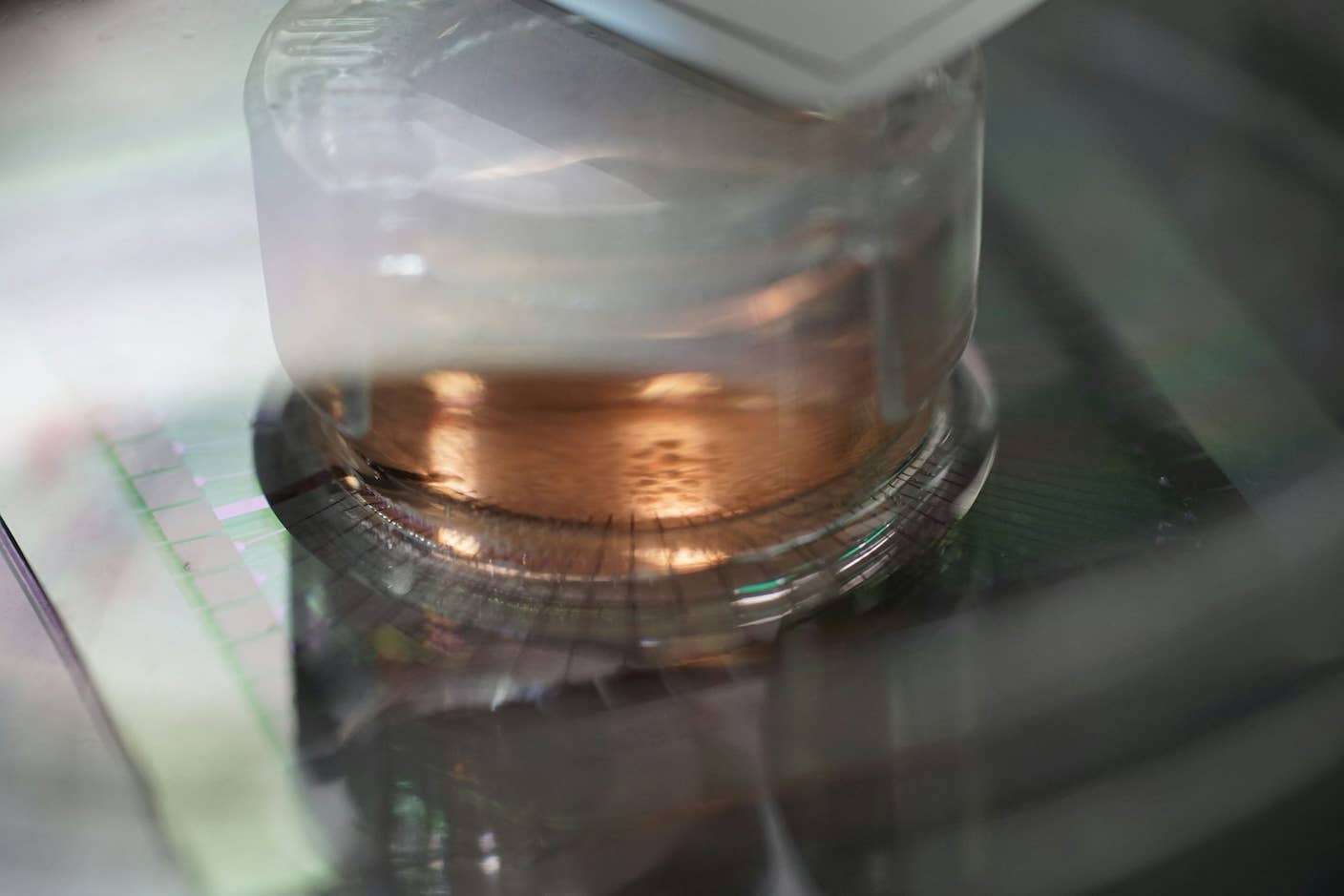
See below an exclusive pic sent to us directly from Dr. Ingber:
[images courtesy of Image: Kristin Johnson/Harvard Medical School/Science]
Drew Halley is a graduate student researcher in Anthropology and is part of the Social Science Matrix at UC Berkeley. He is a PhD candidate in biological anthropology at UC Berkeley studying the evolution of primate brain development. His undergraduate research looked at the genetics of neurotransmission, human sexuality, and flotation tank sensory deprivation at Penn State University. He also enjoys brewing beer, photography, public science education, and dungeness crab. Drew was recommended for the Science Envoy program by UC Berkeley anthropologist/neuroscientist Terrence Deacon.
Related Articles
Scientists Send Secure Quantum Keys Over 62 Miles of Fiber—Without Trusted Devices
This Light-Powered AI Chip Is 100x Faster Than a Top Nvidia GPU
How Scientists Are Growing Computers From Human Brain Cells—and Why They Want to Keep Doing It
What we’re reading