Researchers in Canada and Sweden have successfully treated corneal damage by implanting human collagen into patient’s eyes. According to results recently published in Science Translational Medicine, 10 Swedish patients received biosynthetic corneas crafted from collagen and were monitored for 24 months as part of a phase I clinical trial. Cells from the patients (including nerve cells) grew onto the collagen, allowing for natural tearing, and 6 saw noticeable improvements in vision. The work was spear headed by May Griffith of the Ottawa Hospital Research Institute and surgery was led by Per Fagerholm of Linkoping University in Sweden. Millions of people around the world could have their vision restored by this new material, and it represents a significant step towards regenerating the eye.
For the millions who have lost vision due to corneal damage, transplants are generally the most successful solution. Yet we have a severe shortage of available corneas as they are typically only harvested from recently deceased patients and require matching between donor and recipient. A synthetic cornea is needed until we can find a non-surgical solution. In the beginning of the summer we discussed a remarkable new polymer cornea developed in Germany that will soon be available to patients in the EU. That completely artificial cornea is set to help thousands in the next year, while this collagen cornea from Canada is still in clinical trials. Why then should we be interested in this biosynthetic version?
Natural cell growth. While the polymer cornea allows cells to grow into its edges (this is one of its very useful properties) it does not allow cells into its center. This would cloud the device. The collagen cornea, in contrast, acts as a sort of scaffold so that the patients cells can grow into and on it, forming a quasi-natural corneal tissue layer. In other words, the polymer cornea is a cool piece of plastic that the eye accepts, while the collagen cornea more actively integrates itself into the eye. Griffith and Fagerholm’s work shows that blood vessel and nerve cells move onto the collagen. This allows the biosynthetic cornea to become sensitive to touch. Tears form naturally. I should mention that both materials (polymer and collagen) do not require donor/recipient matching. The polymer is a plastic not rejected by the body. The collagen, though human in origin, doesn’t invoke an immune response.
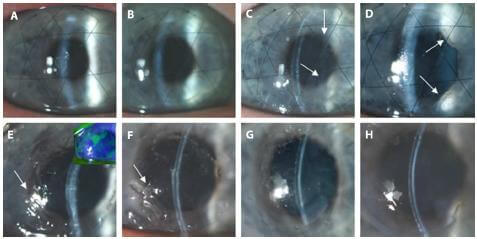
I don’t want to underplay the significance of the polymer cornea. It a viable means of restoring vision to thousands that’s here today (more or less). Nor do I want to over-hype the collagen cornea – cell integration is far from perfect. In fact, we should still be skeptical at this point because trial size was small (as normal for phase I) and results were good but not great – 60% success rate for improved vision.
Instead I would like to place these two projects in a spectrum of synthetic corneas. The polymer is an immediate solution that is likely to remain cutting edge for years to come. Then it is likely the collagen technology will be ready and will provide a more complete healing solution that relies more on the eye’s own cells. Finally we’ll want a means to have the eye completely regenerate itself, likely through the use of stem cells (we’ve seen work in this area already). Each of these technologies is a valuable part of that spectrum of cures for corneal blindness.
The use of collagen scaffolding is a very promising technology. We’ve seen it used to promote stem cell growth for complex organs in rodents, and it’s enabled a child to grow a new trachea in his throat! Now we’re seeing a similar technique applied to eye repair. I’m very excited to see how this concept can be adapted to other areas of the body. Eventually it may be part of the system used to encourage our bodies to regenerate themselves by promoting natural stem cell growth. It is likely to take years before the collagen cornea becomes a widespread means for restoring sight, but it’s already hinting at the potential for new technique that could help return vision to millions.
[image credits: Ottawa Hospital Research Institute, Fagerholm et al Sci. Transl. Med. 2010]
[source: OHRI News, Fagerholm et al Sci. Transl. Med. 2010, Fagerholm et al Clinical and Translational Science 2009]


