We’re much better at saving the lives of those who suffer a heart attack these days. Sadly, many people survive a heart attack only to later succumb to heart failure from the damage it caused. Modern methods help heal the heart somewhat after a heart attack, but cardiologists think stem cell therapy might one day offer a far superior alternative.
Stem cells aren’t just good for growing new organs, they can also heal old or damaged ones from the inside. Thousands of patients whose hearts were damaged in a heart attack have undergone some form of stem cell therapy worldwide, and the results are promising. But there’s a problem. Once in the heart, the cells don’t tend to stay put.
Dr. W. Robert Taylor, professor of medicine at Emory and Georgia Tech and director of Emory’s cardiology division, recently co-authored a paper on a new technique that may significantly increase the efficacy of stem cell therapy in the heart.
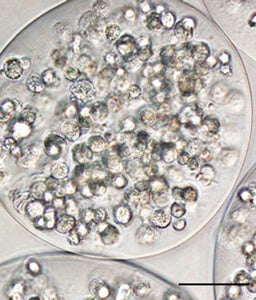
The new procedure, tested in mice, encapsulates stem cells in alginate, a gummy substance derived from algae and used widely (and safely) in human products. Thus confined, the cells stick around longer and deliver greater healing to the heart muscle.
Dr. Taylor told Singularity Hub that current methods attempt to repair damaged parts of the heart by reintroducing blood flow using stents, surgery, or clot-busting drugs.
“While there are great benefits from these approaches, and great strides have been made in decreasing mortality and morbidity from heart attacks, these approaches do not regenerate new tissue or grow new blood vessels. They essentially mitigate the damage.”
Stem cells release hormones and proteins to stimulate growth of new muscle and blood vessels. But the heart is an inhospitable environment, and the forces therein act on implanted cells like “fingers squeezing slippery watermelon seeds.” Some studies indicate the cells disappear in just a few hours.
“It just makes sense that if many of the cells that you administer either die or are expelled from the beating heart, then the efficacy is limited.”
The new encapsulation method makes the whole process far more productive. By keeping the cells together, you keep them happy. And the longer they’re happy and producing, the more healing action you’ll see. Dr. Taylor said, “We saw about a 50% reduction in the damage to the heart after a heart attack.”
Patients would eventually supply their own stem cells for the therapy. The researchers used a particular variety that are readily available in bone marrow, fat, and other tissues. The current procedure requires surgery, but further refinements may allow the cells to be delivered by catheter or needle.
More study is required in larger animals and eventually humans to prove the method is consistently effective and safe. Even so, Dr. Taylor is optimistic.
“One of the exciting aspects of this work is the ability to translate this to humans. Alginate is currently used in many other applications. We anticipate that the hurdles to human studies are relatively modest.”
Stem cell retention is not just problematic in heart therapies. Dr. Taylor noted it is a major problem in the field generally. The team has also used the encapsulation method to treat damage related to vascular disease—and they plan to launch human trials there first.
“We are hoping to get funding to move this forward in humans in the near future,” he said.
Image Credit: HealthGauge/Flickr; Cellular Encapsulation Enhances Cardiac Repair, Rebecca D. Levit, et. al., J Am Heart Assoc. 2013



