No lethal pandemic lasts forever. The 1918 flu, for example, crisscrossed the globe and claimed tens of millions of lives, yet by 1920, the virus that caused it had become significantly less deadly, causing only ordinary seasonal flu. Some pandemics have lasted longer, like the Black Death, which swept out of Central Asia in 1346, spread across Europe, and ultimately may have killed as many as a third of the inhabitants of Europe, the Middle East, and parts of Asia. That pandemic, too, came to an end, roughly seven years after it started, probably because so many had perished or developed immunity.
As far as scientists and historians can tell, the bacterium that caused the Black Death never lost its virulence, or deadliness. But the pathogen responsible for the 1918 influenza pandemic, which still wanders the planet as a strain of seasonal flu, evolved to become less deadly, and it’s possible that the pathogen for the 2009 H1N1 pandemic did the same. Will SARS-CoV-2, the virus that causes Covid-19, follow a similar trajectory? Some scientists say the virus has already evolved in a way that makes it easier to transmit. But as for a possible decline in virulence, most everyone says it’s too soon to tell. Looking to the past, however, may offer some clues.
The idea that circulating pathogens gradually become less deadly over time is very old. It seems to have originated in the writings of a 19th-century physician, Theobald Smith, who first suggested that there is a “delicate equilibrium” between parasite and host, and argued that, over time, the deadliness of a pathogen should decline since it is really not in the interest of a germ to kill its host. This notion became conventional wisdom for many years, but by the 1980s, researchers had begun challenging the idea.
In the early 1980s, the mathematical biologists Roy Anderson and Robert May, proposed that germs transmit best when hosts shed a lot of the pathogen, which may often mean when they are quite sick. If you’re really sick, you are—the argument goes—shedding lots of virus, which makes it easier for the next host to pick it up. So virulence and transmissibility go hand in hand, until the germ gets so deadly it winds up killing its host too soon, and therefore can’t spread at all. This is known as the transmission-virulence trade-off. The most familiar example is that of the myxoma virus, a pathogen introduced to Australia in 1950 to rid the country of rabbits. Initially, the virus killed more than 90 percent of Australian rabbits it infected. But over time, a tense truce developed: Rabbits evolved resistance, the myxoma germ declined in virulence, and both rabbits and germ remained in precarious balance for some time.
A second theory, developed by evolutionary epidemiologist Paul Ewald, which he calls the “theory of virulence,” suggests that, as a rule, the deadlier the germ, the less likely it is to spread. The reason: If victims are quickly immobilized (think of Ebola, for example), then they can’t readily spread the infection. By this thinking, if a germ requires a mobile host to spread, its virulence will, of necessity, decline. Like the older conventional wisdom, the theory of virulence recognizes that many germs will evolve less virulence as they circulate and adapt to the human population. But Ewald’s theory also proposes that germs all have their own strategies to spread, and some of those strategies allow the germ to maintain high virulence and transmissibility.
Durability, Ewald says, is one such strategy. Variola virus, which causes smallpox, is very durable in the external environment, and it can have a high death rate of 10 to 40 percent. Ewald calls it and other durable germs “sit-and-wait” pathogens. Some deadly infections are spread from very sick hosts by vectors: fleas, lice, mosquitos, or ticks. Others, such as cholera, are spread in water. Still others, such as hospital-acquired staph infections, are spread by people taking care of the sick or dying. This is what happened in the women’s hospitals of the 19th century, when doctors spread puerperal or “childbed” fever from one postpartum woman to another.
All of these strategies, according to Ewald, may prevent a germ’s otherwise inevitable slide to lower virulence.
….
So what do these evolutionary theories suggest about SARS-CoV-2 and its likely trajectory? Is the novel coronavirus likely to decline in virulence as it cycles from person to person across the world?
SARS, an earlier outbreak of a serious coronavirus that disrupted the world from 2002 to 2003, offers an interesting contrast. That virus seemed to spread late in the course of infection from people who were very sick, and it eventually infected around 8,000 people, killing 774 before being driven out of existence by a hard-fought global effort to isolate sick patients. But SARS-CoV-2, researchers know, is transmissible early in the infection. There is no necessary relationship between transmissibility and severity. Even asymptomatic cases may shed significant amounts of virus, and there doesn’t necessarily seem to be an increased risk with exposure to sicker people.
It seems unlikely, therefore, that the course of SARS-CoV-2 evolution will strictly reflect Anderson and May’s transmission-virulence trade-off model. To predict SARS-CoV-2’s evolutionary trajectory, Ewald looks to the durability of the virus instead. He points out that SARS-CoV-2 infectious particles last on various surfaces between hours and days, making it approximately as durable as influenza virus. He argues, therefore, that SARS-CoV-2 is likely to evolve virulence to levels much like that of seasonal influenza, with a typical death rate of 0.1 percent.
But there’s still no way to be certain that’s the course SARS-CoV-2 will take. And even the current death rate is uncertain because differences in testing for the coronavirus from country to country make a complete accounting of global infections impossible.
Still, scientists might have already observed evolutionary change in the virus, though apparently in the direction of increased transmissibility, not of lower virulence. A team led by Bette Korber, a computational biologist at Los Alamos National Laboratory, published a paper in the journal Cell in July showing that a strain carrying a mutation identified as D614G appeared to be replacing the initial strain that first emerged out of Wuhan, China. Korber and her team suggested that, on the basis of their research—conducted in cells in culture—the new strain seemed to be more infectious than the original. While the paper notes in its limitations that “infectiousness and transmissibility are not always synonymous,” Korber says the findings are consistent with higher transmissibility.
As with an earlier version of the study shared prior to peer review in April, this conclusion was soon subjected to a barrage of criticism: The replacement that Korber had taken for evidence that the change had been selected for, others ascribed to accident or to other evolutionary processes. Echoing a limitation noted in the Cell paper, critics further emphasized that cell culture studies aren’t able to replicate the complexities of real life, so results should be interpreted with caution. Shortly after the Cell paper was published, Yale epidemiologist and virologist Nathan Grubaugh told National Geographic, “There is a huge gap between infectiousness in a lab and human transmission.”
Neither Grubaugh nor his colleague Angela Rasmussen, a virologist at Columbia University who has also expressed skepticism regarding the mutation’s impact on transmissibility, responded to requests for comment.
But time has shown—and scientists including Grubaugh agree—that this new strain is now the primary one. As Korber puts it: “The D614G strain is now the pandemic. You can hardly even sample the [original] Wuhan virus anymore. In early March, the virus was a different virus than it is today.” This near-complete replacement of the original strain indicates that selection—likely selection toward greater transmissibility—was responsible for the shift, says Korber.
According to Ewald’s analysis, high transmissibility is often associated with lower virulence. He expects to see evidence that SARS-CoV-2 is evolving in that direction. Still, right now, it’s hard to tease apart this kind of viral evolution from improvements in testing, treatment, and social distancing. SARS-CoV-2 testing, for instance, is more accessible than it was earlier in the pandemic. This means patients are hospitalized and treated sooner, offering a better chance at survival, wrote Cameron Wolfe, an infectious disease physician and researcher at Duke University who treats many Covid-19 patients, in an email. Further, he wrote, experimental treatments might be helping hospitalized patients, while some of the most vulnerable people—those in nursing homes—are now better protected from exposure.
“Everyone talks about viral evolution” potentially leading to decreased mortality, wrote Wolfe. “But I haven’t seen any conclusive data to support that hypothesis yet.”
….
Like plague, Covid-19 is a stealth infection, and that might ultimately slow evolution toward lower virulence. Yersinia pestis, the germ that causes plague, tamps down the early immune response, so that infected people can travel and spread infection for days before they feel sick. Similarly, people infected with SARS-CoV-2 seem capable of infecting others before experiencing any symptoms. This sly mode of viral spread may make the evolution of lower virulence less likely, as infected but asymptomatic people are the perfect mobile viral delivery systems.
Yet even without an evolutionary process pushing SARS-CoV-2 towards lower virulence, over time, the virus might affect people differently, said Columbia University virologist Vincent Racaniello. “SARS-CoV-2 may become less deadly, not because the virus changes, but because very few people will have no immunity,” he said. In other words, if you’re exposed to the virus as a child (when it doesn’t seem to make people particularly sick) and then again and again in adulthood, you’ll only get a mild infection. Racaniello points out that the four circulating common cold coronaviruses “all came into humans from animal hosts, and they may have been initially quite virulent.” Now, he says, they infect 90 percent of children at young ages. At later ages, all you get is the common cold.
Compared to influenza viruses, coronaviruses are more stable and less likely to evolve in response to pre-existing immunity. As a result, many experts argue, safe and effective vaccines remain the best chance for escaping the maze of Covid-19 infection. Regular boosters may be necessary as the virus cycles, not because the virus is rapidly evolving, but because human immunity may wane.
Such an outcome would mark the end of this current pandemic. Yet even then, experts believe, some version of the virus will continue to circulate, perhaps as a common cold virus or an occasional deadly outbreak among the unvaccinated, for many years, if not forever.
This article was originally published on Undark. Read the original article.
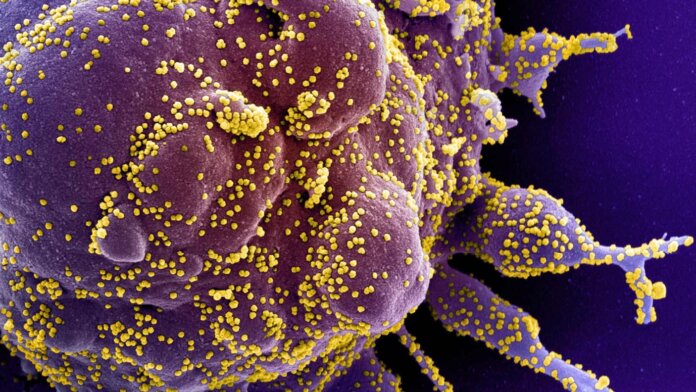
Image credit: Electron microscope image of a human cell (purple) heavily infected with SARS-CoV-2 virus particles (yellow) courtesy of National Institute of Allergy and Infectious Diseases / NIH