Moonshot Project Aims to Understand and Beat Cancer Using Protein Maps

Share
Understanding cancer is like assembling IKEA furniture.
Hear me out. Both start with individual pieces that make up the final product. For a cabinet, it’s a list of labeled precut plywood. For cancer, it’s a ledger of genes that—through the Human Genome Project and subsequent studies—we know are somehow involved in cells mutating, spreading, and eventually killing their host.
Yet without instructions, pieces of wood can’t be assembled into a cabinet. And without knowing how cancer-related genes piece together, we can’t decipher how they synergize to create one of our fiercest medical foes.
It’s like we have the first page of an IKEA manual, said Dr. Trey Ideker at UC San Diego. But “how these genes and gene products, the proteins, are tied together is the rest of the manual—except there’s about a million pages worth of it. You need to understand those pages if you’re really going to understand disease.”
Ideker’s comment, made in 2017, was strikingly prescient. The underlying idea is seemingly simple, yet a wild shift from previous attempts at cancer research: rather than individual genes, let’s turn the spotlight on how they fit together into networks to drive cancer.
Together with Dr. Nevan Krogan at UC San Francisco, a team launched the Cancer Cell Map Initiative (CCMI), a moonshot that peeks into the molecular “phone lines” within cancer cells that guide their growth and spread. Snip them off, the theory goes, and it’s possible to nip tumors in the bud.
This week, three studies in Science led by Ideker and Krogan showcased the power of that radical change in perspective. At its heart is protein-protein interactions: that is, how the cell’s molecular “phone lines” rewire and fit together as they turn to the cancerous dark side.
One study mapped the landscape of protein networks to see how individual genes and their protein products coalesce to drive breast cancer. Another traced the intricate web of genetic connections that promote head and neck cancer.
Tying everything together, the third study generated an atlas of protein networks involved in various types of cancer. By looking at connections, the map revealed new mutations that likely give cancer a boost, while also pointing out potential weaknesses ripe for target-and-destroy.
For now, the studies aren’t yet a comprehensive IKEA-like manual of how cancer components fit together. But they’re the first victories in a sweeping framework for rethinking cancer.
“For many cancers, there is an extensive catalog of genetic mutations, but a consolidated map that organizes these mutations into pathways that drive tumor growth is missing,” said Drs. Ran Cheng and Peter Jackson at Stanford University, who weren’t involved in the studies. Knowing how those work “will simplify our search for effective cancer therapies.”
Cellular Chatterbox
Every cell is an intricate city, with energy, communications systems, and waste disposal needs. Their secret sauce for everything humming along nicely? Proteins.
Proteins are indispensable workhorses with many tasks and even more identities. Some are builders, tirelessly laying down “railway” tracks to connect different parts of a cell; others are carriers, hauling cargo down those protein rails. Enzymes allow cells to generate energy and perform hundreds of other life-sustaining biochemical reactions.
But perhaps the most enigmatic proteins are the messengers. These are often small in size, allowing them to zip around the cell and between different compartments. If a cell is a neighborhood, these proteins are mailmen, shuttling messages back and forth.
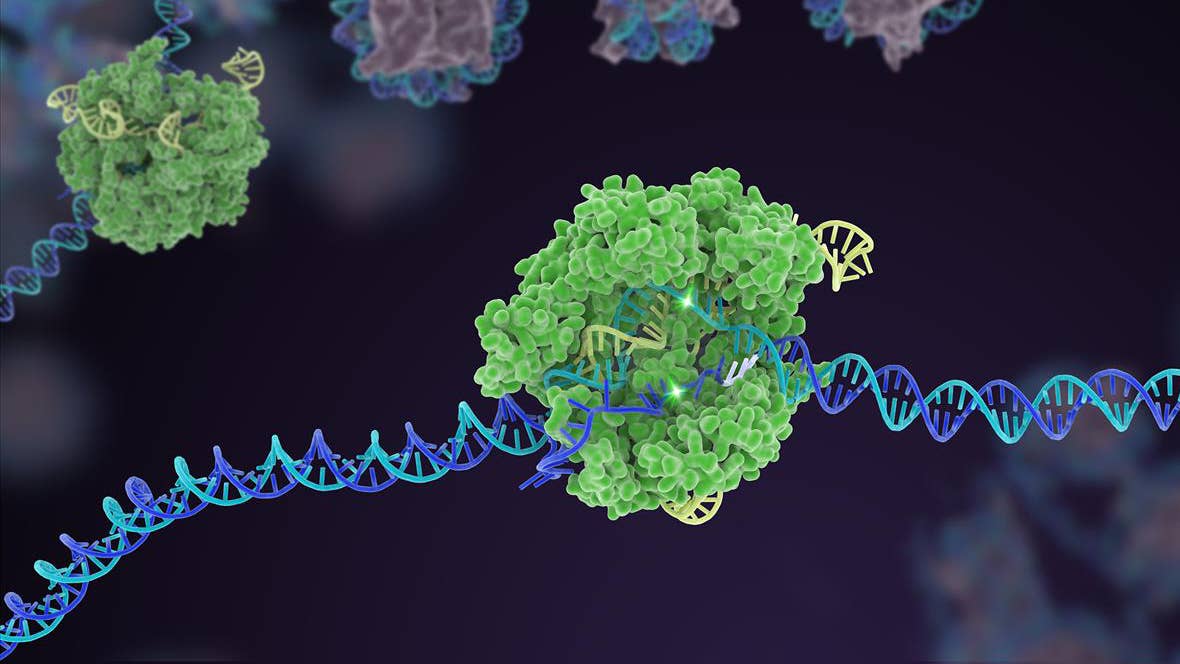
Rather than dropping off mail, however, they deliver messages by physically tagging onto other protein. These “handshakes” are dubbed protein-protein interactions (PPIs), and are critical to a cell’s function. PPIs are basically the cell’s supply chain, communications cable, and energy economy rolled into one massive infrastructure. Destroying just one PPI can lead a thriving cell to die.
PPIs aren’t set in stone. Going back to the mailman analogy, a single protein can have multiple “mail routes,” depending on the status of a cell. Some connections are beneficial: the end result is generating energy or sweeping away cellular garbage. Others not so much, releasing molecular brakes that drive a cell towards a cancerous fate. Disrupt a dangerous PPI, and it’s possible to stop a tumor’s growth or spread in its tracks.
A Protein Pathway Atlas
The new studies tapped into PPIs as a new perspective to understand cancer.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Previous research mainly focused on a cell’s genetic changes as it turns cancerous. Many of those changes alter the cell’s surface landscape. For example, CAR-T, the breakthrough cancer therapy that boosts a person’s own immune cells to better target cancers, relies on tumor-specific markers that dot the surface of a cell to hone in and attack.
The Cancer Cell Map Initiative shifts away from individual genes toward the big picture: let’s monitor a cell’s PPIs, see how these interactions reorganize in cancers, and find new protein players that contribute to cancer.
Enter big data. One study screened roughly 650 proteins in a type of cell involved in head and neck cancer, finding nearly 800 interactions between proteins. Digging deeper, the authors developed an algorithm to fish out cancer-specific interactions, finding a slew of PPIs and protein players in tumors, many of which were previously unknown.
These new cancer drivers seem to activate specific communication pathways, the authors explained. One example is a new protein couple, Daple and FGFR3. By physically binding together, the pair seemed to help tumor cells migrate, suggesting that cutting off their dalliance could potentially reduce the chance of cancer cells spreading.
A separate study took the same approach but focused on breast cancer. Mutation to BRCA1 is a well-known genetic cause for inherited breast cancer risk. The authors screened for proteins that interact with BRCA1, and found a library of candidate proteins that grab onto parts of BRCA1 that tend to mutate. One protein, spinophilin, especially caught the team’s eye. Although previously linked to other types of tumors, it’s never been implicated in breast cancer.
“We’re elevating the conversation about cancer from individual genes to proteins, allowing us to look at how the varying mutations we see in patients can have the same effects on protein function,” said Ideker.
A New Looking Glass
PPIs don’t just exist in cancer cells. They run a whole gamut of cellular functions. Because of their importance, scientists have long documented these interactions in massive databases—a powerful resource, yet largely untapped for cancer research.
“To date, many published PPI studies are ripe for further analysis, but they are often not extensively mined,” said Cheng and Jackson.
That’s set to change. The third study combined data from the previous two works—head and neck cancer and breast cancer—with a broad range of previously reported human PPIs in publicly-available databases. The authors then assigned a score for pairs of human proteins to screen for protein assemblies within a tumor cell type—a bit like mapping solar systems in a galaxy. Overall, they mapped nearly 400 different protein systems in 13 different types of tumors, forming a massive atlas of PPIs. By analyzing those maps, the team found several previously hard-to-detect genetic mutations that can help a cancer spread more easily.
Despite these successes, our PPI cancer maps remain relatively rudimentary, capturing just a fraction of protein handshakes in a cell. They’re also static, whereas PPIs dynamically change, similar to the way neural networks change. However, just a small peek into these new maps already suggests that different types of tumors have a diverse and potentially characteristic set of PPIs, ones different from healthy cells that future cancer treatments could target.
“We’re in the perfect position to take advantage of this revolution on every level,” said Krogan. “I couldn’t be more excited than I am right now. We can do such damage to cancer.”
Image Credit: Free-Photos from Pixabay
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading