Our skin is a natural wonder of bioengineering.
The largest organ in the body, it’s a waterproof defense system that protects against infections. It’s packed with sweat glands that keep us cool in soaring temperatures. It can take a serious beating—sunburns, scratches and scrapes, cooking oil splatters, and other accidents in daily life—but rapidly regenerates. Sure, there may be lasting scars, but signs of lesser damage eventually fade away.
Given these perks, it’s no wonder scientists have tried recreating skin in the lab. Artificial skin could, for example, cover robots or prosthetics to give them the ability to “feel” temperature, touch, or even heal when damaged.
It could also be a lifesaver. The skin’s self-healing powers have limits. People who suffer from severe burns often need a skin transplant taken from another body part. While effective, the procedure is painful and increases the chances of infection. In some cases, there might not be enough undamaged skin left. A similar dilemma haunts soldiers wounded in battle or those with inherited skin disorders.
Recreating all the skin’s superpowers is tough, to say the least. But last week, a team from Wake Forest University took a large step towards artificial skin that heals large wounds when transplanted into mice and pigs.
The team used six different human skin cell types as “ink” to print out three-layered artificial skin. Unlike previous iterations, this artificial skin closely mimics the structure of human skin.
In proof-of-concept studies, the team transplanted the skin into mice and pigs with skin injuries. The skin grafts rapidly tapped into blood vessels from surrounding skin, integrating into the host. They also helped shape collagen—a protein essential for healing wounds and reducing scarring—into a structure similar to natural skin.
“These results show that the creation of full thickness human bioengineered skin is possible, and promotes quicker healing and more naturally appearing outcomes,” said study author Dr. Anthony Atala.
Wait…What’s Full Thickness Skin?
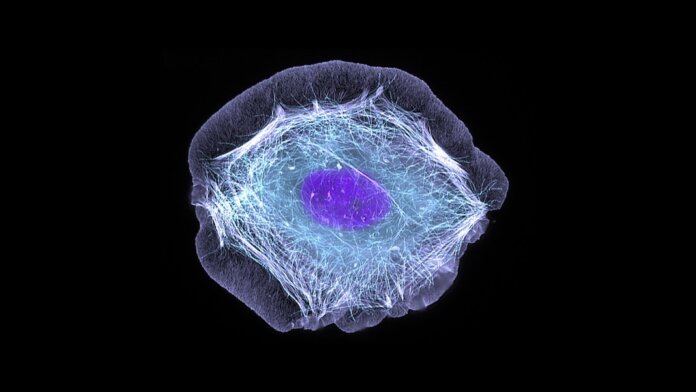
We often picture the skin as a fitted sheet that wraps around the body. But under the microscope, it’s an intricate masterpiece of bio-architecture.
Or I like to think of it as a three-layered cake.
Each layer has different cell types tailored to their distinctive functions. The top layer is the guardian. A direct link to the outside world, it has cell types that can endure UV light, arid weather, and harmful bacteria. It also houses cells that produce pigmentation. These cells continuously shed when damaged and are replaced to keep the barrier strong.
The middle layer is the bridge. Here, blood vessels and nerve fibers connect the skin to the rest of the body. This layer is packed with cells that produce body hair, sweat, and lubricating oils—the bane of anyone prone to acne. As the widest layer, it’s held tightly together by collagen, which gives the skin its flexibility and strength.
Finally, the deepest skin layer is the “puffy coat.” Made primarily of collagen and fat cells, this layer is a shock absorber that protects the skin from injuries and helps maintain body heat.
Recreating all these structures and functions is incredibly hard. Atala’s solution? Three-dimensional bioprinting.
Skin in the Game
Atala is no stranger to bioprinting.
In 2016, his team developed a tissue-organ printer that can print large tissues of any shape. Using clinical data, the team made computer models to guide the printer when printing various bone structures and muscles. A few years later, they engineered a skin bioprinter that used two cell types—from either the top or middle layer—to directly patch injured skin. Though the skin could close large wounds, it only captured part of natural skin’s complexity.
The new study used six types of human cells as bioink, recreating our skin’s architecture top to bottom. To manufacture the artificial skin, the team used computer software to direct the placement of cells in each layer. Called 3D-extrusion printing, the technology uses air pressure to print highly sophisticated tissues out of a nozzle. It sounds complicated, but it’s a bit like squeezing out icing of different colors to decorate a cake.
As a first step, the team suspended cells in a hydrogel made primarily of a liver-secreted protein. Unlike synthetic materials, this body-produced base increases biocompatibility. The team then printed a 3D skin graft, layer by layer, measuring an inch on each side—a bit bigger than a sugar cube.
The bioprinted skin maintained its three layers for at least 52 days in the lab and developed areas with pigmentation and normal shedding.
Encouraged, the team next tested the artificial skin in mice. All wounds treated with the artificial skin grafts completely healed in two weeks, as opposed to those treated with only the hydrogel or letting the wound heal naturally.
The artificial skin was especially good at building the skin’s upper protective layer, forming structures that resembled natural healing. It also produced collagen, and—more importantly—weaved it into a wicker-basket-like structure similar to human skin.
The bioprinted skin further recruited the mice’s own blood vessel cells, generating a network of small vessels inside the graft. Using a stain to track human proteins in the graft, the team found the transplanted cells integrated with their host in the middle layer of the skin.
Squeaking By?
Mice have thinner skin than humans. Pigs’ skins, in contrast, are closer to ours. In a second test, the team scaled up the technology for transplantation in pigs. Here, they harvested four types of cells from pigs through biopsies—including some that make up the skin’s outer layer, collagen, blood vessels, and fatty tissue—and grew them inside a bioreactor for 28 days.
Some batches failed. On average, however, the brew generated enough cells to double the size of the initial graft for greater coverage. The resulting artificial skin patch was roughly the size of the face of a Rubik’s cube and matched the thickness of the pig’s skin.
Like the results in mice, the grafts rapidly closed large wounds without the usual “puckering” effect—where the skin constricts like a grape to a raisin—that leads to scarring.
The team concluded this is likely because the graft amplified genes responsible for wound healing, with some also regulating immune responses that help grow new blood vessels and reduce scarring.
The artificial skin is promising but still in its infancy. When grafted onto pigs, it didn’t reliably produce pigmentation, which could be troubling to those with darker skin tones. The grafts also didn’t produce body hair, though they contained structures for its growth in the bioink. While it might not be the worst (no more shaving!), the results suggest there’s still a lot to learn.
To Atala, the effort’s worth it. “Comprehensive skin healing is a significant clinical challenge, affecting millions of individuals worldwide, with limited options,” he said. The study suggests printing full-scale skin is possible for treating devastating wounds in humans.
Image Credit: A normal skin cell under the microscope. Torsten Wittmann, University of California, San Francisco (via NIH/Flickr)