A Universal Vaccine Against Any Viral Variant? A New Study Suggests It’s Possible

Share
From Covid boosters to annual flu shots, most of us are left wondering: Why so many, so often?
There’s a reason to update vaccines. Viruses rapidly mutate, which can help them escape the body’s immune system, putting previously vaccinated people at risk of infection. Using AI modeling, scientists have increasingly been able to predict how viruses will evolve. But they mutate fast, and we’re still playing catch up.
An alternative strategy is to break the cycle with a universal vaccine that can train the body to recognize a virus despite mutation. Such a vaccine could eradicate new flu strains, even if the virus has transformed into nearly unrecognizable forms. The strategy could also finally bring a vaccine for the likes of HIV, which has so far notoriously evaded decades of efforts.
This month, a team from UC California Riverside, led by Dr. Shou-Wei Ding, designed a vaccine that unleashed a surprising component of the body’s immune system against invading viruses.
In baby mice without functional immune cells to ward off infections, the vaccine defended against lethal doses of a deadly virus. The protection lasted at least 90 days after the initial shot.
The strategy relies on a controversial theory. Most plants and fungi have an innate defense against viruses that chops up their genetic material. Called RNA interference (RNAi), scientists have long debated whether the same mechanism exists in mammals—including humans.
“It’s an incredible system because it can be adapted to any virus,” Dr. Olivier Voinnet at the Swiss Federal Institute of Technology, who championed the theory with Ding, told Nature in late 2013.
A Hidden RNA Universe
RNA molecules are usually associated with the translation of genes into proteins.
But they’re not just biological messengers. A wide array of small RNA molecules roam our cells. Some shuttle protein components through the cell during the translation of DNA. Others change how DNA is expressed and may even act as a method of inheritance.
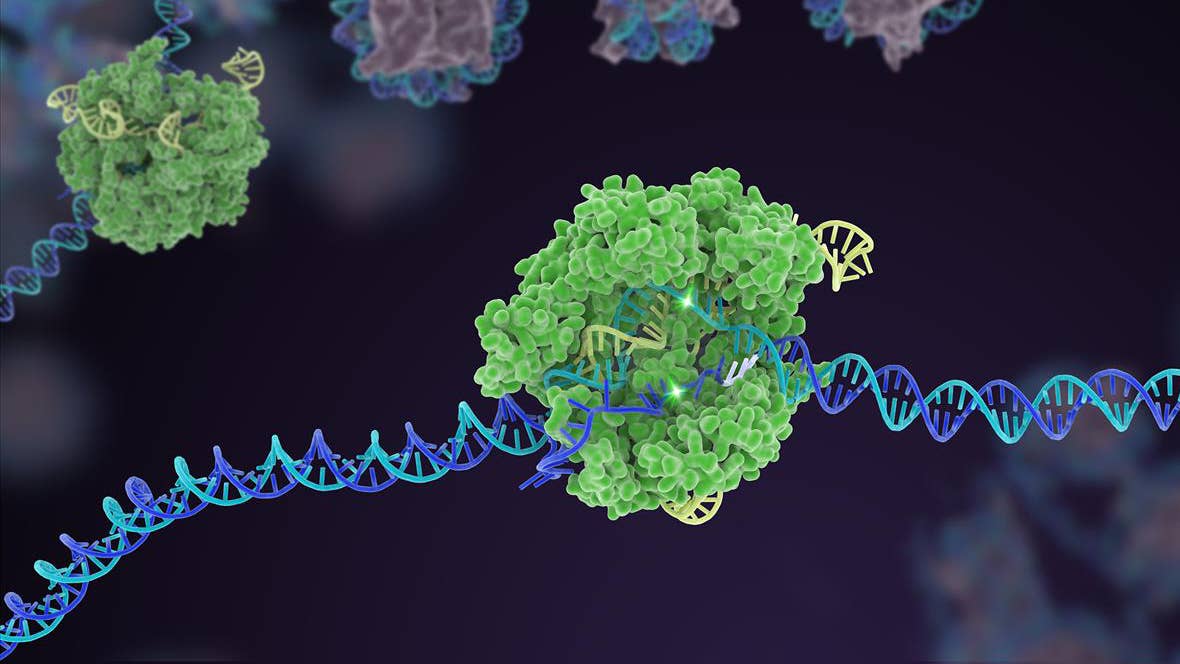
But fundamental to immunity are small interfering RNA molecules, or siRNAs. In plants and invertebrates, these molecules are vicious defenders against viral attacks. To replicate, viruses need to hijack the host cell’s machinery to copy their genetic material—often, it’s RNA. The invaded cells recognize the foreign genetic material and automatically launch an attack.
During this attack, called RNA interference, the cell chops the invading viruses’ RNA genome into tiny chunks–siRNA. The cell then spews these viral siRNA molecules into the body to alert the immune system. The molecules also directly grab onto the invading viruses’ genome, blocking it from replicating.
Here’s the kicker: Vaccines based on antibodies usually target one or two locations on a virus, making them vulnerable to mutation should those locations change their makeup. RNA interference generates thousands of siRNA molecules that cover the entire genome—even if one part of a virus mutates, the rest is still vulnerable to the attack.
This powerful defense system could launch a new generation of vaccines. There’s just one problem. While it’s been observed in plants and flies, whether it exists in mammals has been highly controversial.
“We believe that RNAi has been antiviral for hundreds of millions of years,” Ding told Nature in 2013. “Why would we mammals dump such an effective defense?”
Natural Born Viral Killers
In the 2013 study in Science, Ding and colleagues suggested mammals also have an antiviral siRNA mechanism—it’s just being repressed by a gene carried by most viruses. Dubbed B2, the gene acts like a “brake,” smothering any RNA interference response from host cells by destroying their ability to make siRNA snippets.
Getting rid of B2 should kick RNA interference back into gear. To prove the theory, the team genetically engineered a virus without a functioning B2 gene and tried to infect hamster cells and immunocompromised baby mice. Called Nodamura virus, it’s transmitted by mosquitoes in the wild and is often deadly.
But without B2, even a lethal dose of the virus lost its infectious power. The baby mice rapidly generated a hefty dose of siRNA molecules to clear out the invaders. As a result, the infection never took hold, and the critters—even when already immunocompromised—survived.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


“I truly believe that the RNAi response is relevant to at least some viruses that infect mammals,” said Ding at the time.
New-Age Vaccines
Many vaccines contain either a dead or a living but modified version of a virus to train the immune system. When faced with the virus again, the body produces T cells to kill off the target, B cells that pump out antibodies, and other immune “memory” cells to alert against future attacks. But their effects don’t always last, especially if a virus mutates.
Rather than rallying T and B cells, triggering the body’s siRNA response offers another type of immune defense. This can be done by deleting the B2 gene in live viruses. These viruses can be formulated into a new type of vaccine, which the team has been working to develop, relying on RNA interference to ward off invaders. The resulting flood of siRNA molecules triggered by the vaccine would, in theory, also provide some protection against future infection.
“If we make a mutant virus that cannot produce the protein to suppress our RNAi [RNA interference], we can weaken the virus. It can replicate to some level, but then loses the battle to the host RNAi response,” Ding said in a press release about the most recent study. “A virus weakened in this way can be used as a vaccine for boosting our RNAi immune system.”
In the study, his team tried the strategy against Nodamura virus by removing its B2 gene.
The team vaccinated baby and adult mice, both of which were genetically immunocompromised in that they couldn’t mount T cell or B cell defenses. In just two days, the single shot fully protected the mice against a deadly dose of virus, and the effect lasted over three months.
Viruses are most harmful to vulnerable populations—infants, the elderly, and immunocompromised individuals. Because of their weakened immune systems, current vaccines aren’t always as effective. Triggering siRNA could be a life-saving alternative strategy.
Although it works in mice, whether humans respond similarly remains to be seen. But there’s much to look forward to. The B2 “brake” protein has also been found in lots of other common viruses, including dengue, flu, and a family of viruses that causes fever, rash, and blisters.
The team is already working on a new flu vaccine, using live viruses without the B2 protein. If successful, the vaccine could potentially be made as a nasal spray—forget the needle jab. And if their siRNA theory holds up, such a vaccine might fend off the virus even as it mutates into new strains. The playbook could also be adapted to tackle new Covid variants, RSV, or whatever nature next throws at us.
This vaccine strategy is “broadly applicable to any number of viruses, broadly effective against any variant of a virus, and safe for a broad spectrum of people,” study author Dr. Rong Hai said in the press release. “This could be the universal vaccine that we have been looking for.”
Image Credit: Diana Polekhina / Unsplash
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading