In First Human Trial, Zombie Cancer Cells Train the Body to Fight Tumors
A small trial is testing a decades-old method that transforms cancer cells into a "vaccine" to prevent recurrence.
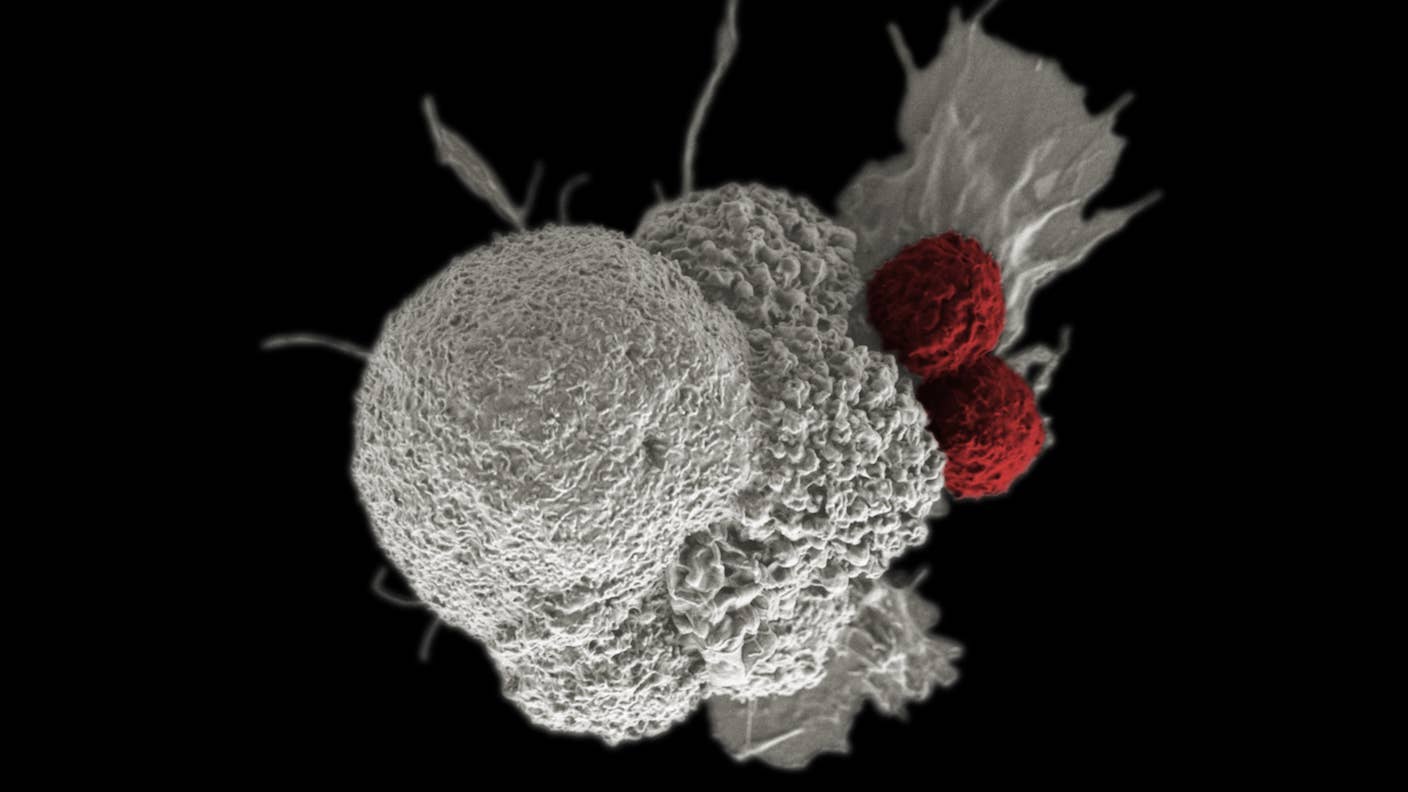
Image Credit
T cells (red) attack cancer cell (white) / Rita Elena Serda, Duncan Comprehensive Cancer Center at Baylor College of Medicine, National Cancer Institute, NIH
Share
Lights, vitamin, action. A combination of vitamin B2 and ultraviolet light hardly sounds like a next-generation cancer treatment. But a small new trial is testing the duo in people with recurrent ovarian cancer.
Led by PhotonPharma, this first-in-humans study builds on decades of work investigating whether we can turn whole cancer cells into “vaccines.” Isolated from cancer patients, the cells are stripped of the ability to multiply but keep all other protein signals intact. Once reinfused, the cells can, in theory, alert the immune system that something is awry.
Known as the Mirasol process, the approach was originally used to neutralize bacteria, viruses, and other pathogens in donated blood or plasma (the yellowish liquid part of blood). But a chance discovery led Ray Goodrich at Colorado State University to re-envision the method as a cancer treatment. White blood cells, he noticed, retained their structure but were inactivated after going through the process, turning into “zombies” that couldn’t divide or function.
Cancer cells disabled in the same way could train the immune system to recognize and attack the real tumor. Researchers pursuing the idea have already used it to keep recurrent cancers at bay in mice and dogs. Encouraged, Goodrich, who helped develop the Mirasol process, co-founded PhotonPharma to bring the treatment to people.
To be clear, the method doesn’t prevent cancer. It’s designed to keep pesky cancer cells from returning. The trial is set to begin early this year at City of Hope, a national cancer research and treatment center, in six patients to gauge safety.
"We are thrilled to have reached this pivotal moment in our journey toward providing a novel treatment option for patients facing advanced ovarian cancer,” said Goodrich in a press release after being given the green light by the FDA to conduct the trial.
A Long Journey
Cancer immunotherapies have come a long way. The blockbuster CAR T cell therapy, for example, has transformed treatment for deadly blood cancers. Here, T cells are removed from the patient and genetically engineered to more effectively recognize cancers. When infused back into the body, these enhanced cells can better hunt down and destroy their targets.
CAR T is a breakthrough, but it’s tough on an already fragile body. Patients undergo a short bout of chemotherapy or radiation to remove existing T cells. This step makes space for the newly engineered cells and reduces competition with existing immune cells. Scientists are working on ways to skip the process, such as a gene-editing injection that transforms T cells inside the body. But even these newer methods still struggle to tackle solid tumors, including ovarian cancer.
Cancer vaccines are also on the rise thanks to mRNA technology. Like Covid vaccines, these shots wake up a sluggish immune system and help immune cells penetrate the formidable barriers surrounding cancer cells.
The Mirasol process is different. Before boosting the immune system, it first neuters cancer cells.
Goodrich began working to purify donated blood during the HIV epidemic in the late 1980s, when contamination was a big concern. It took a decade, but he eventually found a curious duo: Vitamin B2, or riboflavin, and ultraviolet (UV) light. Riboflavin latches onto DNA and RNA molecules, and a blast of UV light damages the genetic material in pathogens, rendering them incapable of growth and reproduction. This essentially cleanses the blood. The process can be conducted in a machine the size of desktop printer and is approved in multiple countries in Europe and Canada.
But the technology is more sledgehammer than scalpel. It also damages red blood cells, platelets, and plasma proteins. To his surprise, however, Goodrich noticed some white blood cells remained intact, though they could no longer replicate. It was this observation that led him to test the procedure on cancer cells.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Using whole cancer cells as vaccines isn’t a new idea. For decades, scientists have tried to use patient’s own tumors to ignite the immune system, often incapacitating them with radiation. Some tests made it to clinical trials for prostate cancers and other solid tumors. But the overall immune response was weak, and the idea soon lost support.
Still, whole cancer cells do have a leg up compared to current immunotherapies. Such treatments use only a small handful of proteins, called neoantigens, to help the immune system identify cancer cells. With Mirasol, the inactivated cancer cells retain all their neoantigens. In theory, this could more effectively alert the immune system: More danger signals should provoke a fiercer response. Using whole cancer cells also means scientists don’t need to spend time figuring out the best neoantigens to include in their treatment.
Unlike CAR T, the inactivated cancer cells can be infused back into patients without radiation or chemotherapy conditioning. And because they can no longer divide, there’s little chance of them growing into new tumors.
Early trials in dogs with solid tumors were promising. In an 11-year-old goldendoodle named Ella, cancer of the liver had spread into surrounding healthy tissue. This made it difficult to completely remove. Rather than resorting to chemotherapy, her owner opted for Goodrich’s experimental process. After treatment, the cancer showed no signs of returning for three years, at which point she passed from health issues unrelated to cancer.
The new trial will treat people with recurrent, advanced ovarian cancer and no other options.
“Traditionally, it’s been chemotherapy, but in 80 percent of those patients who get surgery and chemotherapy, it comes back…we know it’s really not curable at that point,” Mihae Song, a gynecologic oncologist at City of Hope, told The Colorado Sun.
The trial will primarily measure safety. The team will remove cancer cells from patients, inactivate them with UV light and riboflavin, and add several molecules commonly used in vaccines to boost the immune response. Each person will receive three doses of the cells, as the team watches out for side effects and gauges the response.
If it works, Goodrich and team want to recruit more participants and potentially expand the treatment to other types of solid tumors. But success isn’t guaranteed. Tumors eventually suppress immune attacks, and it’s unclear if UV-treated decoys can restore immune cell vigor.
Still, the trial offers an alternative way to tackle stubborn cancers. “You would always hope, but I think it’s too optimistic to think that it completely cures it,” Goodrich told The Colorado Sun. “But it’s maybe something that could add years of life, of good-quality life, onto someone’s lifespan who is diagnosed with this, because, again, the prognosis right now is not very good.”
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles

Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading