RNA-Based Drug Offers New Hope To Hepatitis C Patients
A new drug may present a way for patients to rid their bodies of infection without being subjected to the same severe side effects as current treatments.

Share
About 170 million people in the world suffer from chronic hepatitis C, a viral infection that often leads to cirrhosis or cancer of the liver. Right now, modern medicine can cure about 50 to 80 percent of hepatitis C cases, but often the treatments have side effects that are themselves very harmful. A new drug may present a way for patients to rid their bodies of infection without subjecting to the same harsh side effects.
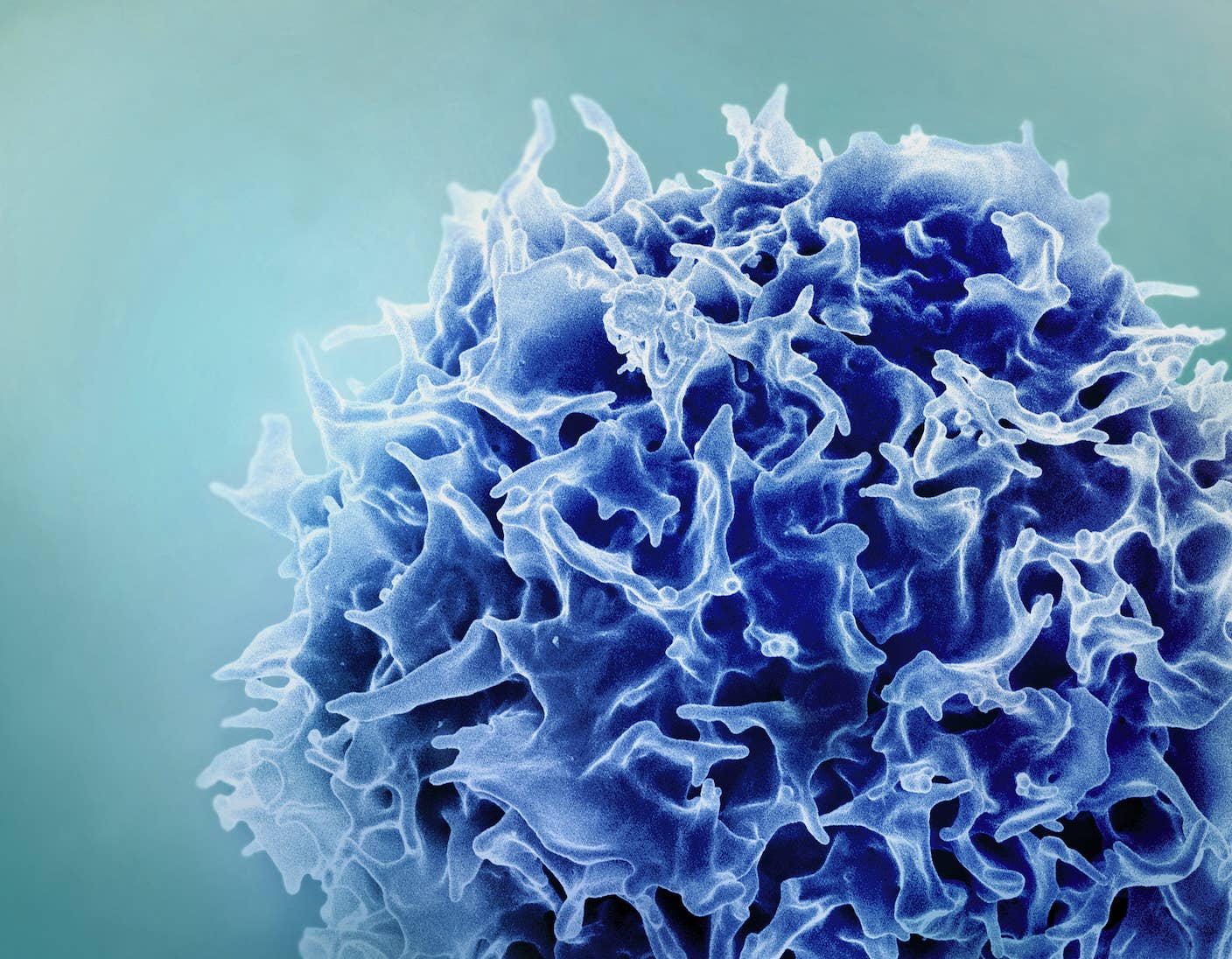
Developed by Santaris Pharma A/S headquartered in Denmark, miravirsen is part of a class of drugs known as RNA interference (RNAi) drugs. RNAi works differently than traditional antivirals that target and disable proteins or other parts of the virus. RNAi drugs are not toxic chemicals but small pieces of the single-stranded RNA molecules that binds other RNA molecules. And rather than disrupting the function of the virus, miravirsin works by binding an RNA molecule in the host cell nucleus that hepatitis C needs to replicate. Without replicating and spreading through the body, the viral infection will be short-lived. This kind of “mopping” up of host cell resources that the virus needs have led some to dub miravirsen the “sponge drug.”
In this phase 2 trial, the goal was to see how much miravirsin was needed to temporarily halt the hepatitis C virus. Three different doses and a placebo were given weekly among 36 patients with chronic hepatitis C over a month. The effects were dose dependent, with viral levels in five out of nine patients receiving the highest dose rendered undetectable. According to Harry Janssen, the study’s lead author, the results are comparable to current hepatitis C treatments. Four of these five patients, however, showed a rebound in their viral levels when the study was concluded 18 weeks later, indicating that a treatment with lasting effects will likely need to be longer than five weeks.
The current study, published in the April 4 issue of The New England Journal of Medicine, was meant to determine an effective dose for miravirsin, as well as evaluate its safety. A much larger study will be needed to determine its overall effectiveness. And while longterm side effects still remain a possibility, the observed short-term side effects were minimal, consisting only of a rash and pain at the site of injection.
![Miravirsin binds to a molecule in host cells called miR-122 that the hepatitis C virus needs to replicate. [Source: Santaris Pharma A/S]](https://singularityhub.com/wp-content/uploads/2013/04/image1A1.jpg)
Miravirsin binds to a molecule in host cells called miR-122 that the hepatitis C virus needs to replicate. [Source: Santaris Pharma A/S]
For one group in the United States, hepatitis C is a big problem. About 2 million baby boomers – those born between 1945 and 1965 – have hepatitis C. They make up about 27 percent of the US population, yet account for three-quarters of all hepatitis C cases in the US. It’s thought that the majority of baby boomers contracted infections during the 70s and 80s, when the spread of hepatitis was at its peak. The disproportionate number of cases for the group prompted the Center for Disease Control to issue a recommendation last August that baby boomers be tested regularly for hepatitis C.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


There are five types of hepatitis, A thru E. Types B and C are of special concern as they have led to chronic diseases for hundreds of millions around the world and combined are the most common cause of liver cirrhosis and cancer. For about 75 to 85 percent of people who contract hepatitis C, the infection becomes a chronic disease.
Since its discovery in 1998, scientists have been trying to use RNAi to halt the ability of viruses to hijack host cell machinery in order to replicate. But for all the hope it had inspired, the path from idea to actual treatment turned out to be much more difficult to traverse than companies had hoped it would be. In 2006 pharmaceutical giant Merck bought Sirna Therapeutics, the San Francisco-based pioneer in making RNAi-based drugs. In 2010 Roche ended its $500 million program to develop RNAi-based drugs. Months before, Novartis opted to not spend the $100 million needed to continue a partnership with the Cambridge, Massachusetts-based RNAi leader, Alnylam. It seemed that, while making the RNA molecules is easy enough, delivering the notoriously fragile molecules to their target cells has proven harder than expected.
But things may be turning around for the as yet unproven technology. Earlier this year the first RNAi-based treatment received FDA approval. Kynamro will be used to treat people with homozygous familial hypercholesterolemia, a rare condition that causes high cholesterol due to the body’s inability to remove low density lipoproteins (“bad” cholesterol, although see here) from blood. The RNAi's in Kynamro work by limiting the body’s ability to produce lipid particles that a processed to become LDLs. In a clinical trial the treatment decreased levels of LDL by 25 percent.
The most common way to treat hepatitis C is with antivirals combined with interferon, a protein that boosts the body’s immune system and slows virus replication, and ribavirin, an antiviral that helps slow the spread of the virus in the body. A major drawback from the current treatment are its side effects that include flu-like symptoms, fatigue, depression, anxiety, diarrhea and nausea. If its phase 3 trial looks anything like its phase 2, miravirsen could be the next RNA-based therapy to get FDA approval and not only help rid patients of infection, but spare them severe side effects at the same time.
Peter Murray was born in Boston in 1973. He earned a PhD in neuroscience at the University of Maryland, Baltimore studying gene expression in the neocortex. Following his dissertation work he spent three years as a post-doctoral fellow at the same university studying brain mechanisms of pain and motor control. He completed a collection of short stories in 2010 and has been writing for Singularity Hub since March 2011.
Related Articles
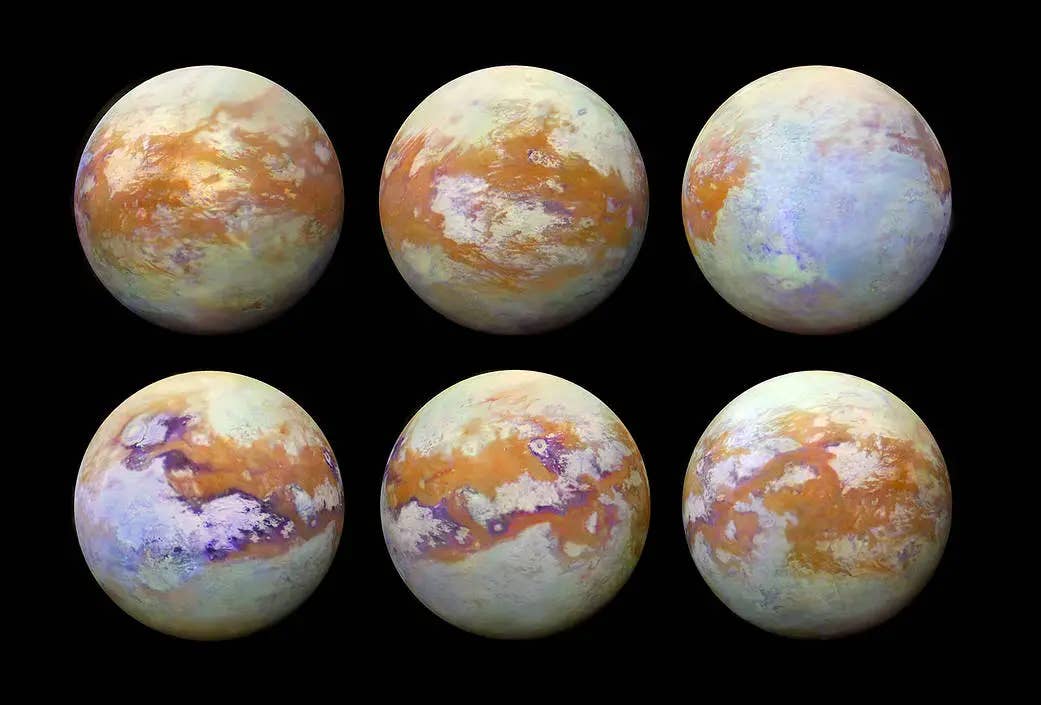
Single Injection Transforms the Immune System Into a Cancer-Killing Machine
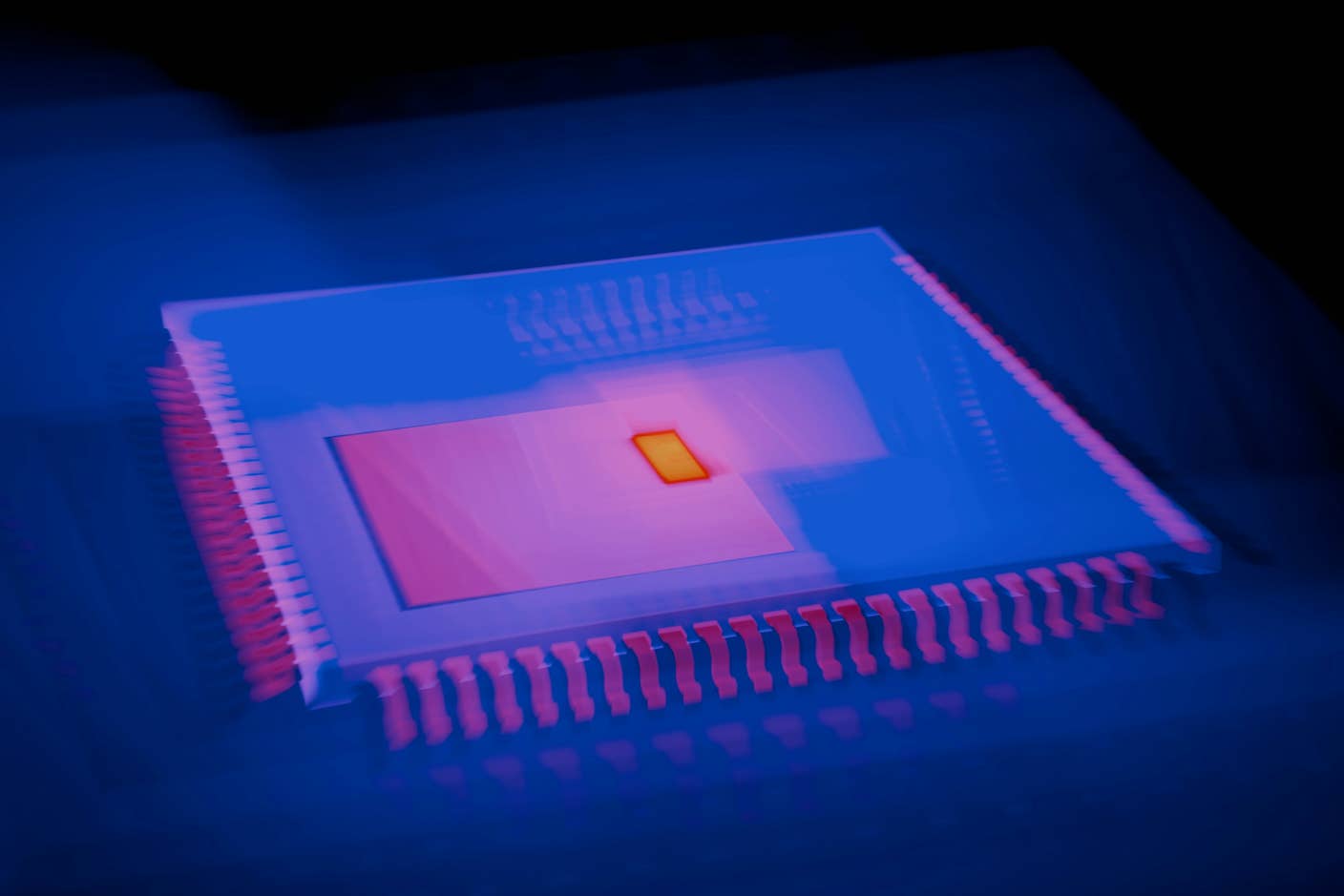
This Light-Powered AI Chip Is 100x Faster Than a Top Nvidia GPU
This Week’s Awesome Tech Stories From Around the Web (Through December 20)
What we’re reading
![RNA molecule folded back upon itself [Source: Wikipedia]](https://singularityhub.com/wp-content/uploads/2013/04/image3A1.jpg)