First Human CRISPR Trial in the US Aims to Cure Inherited Blindness

Share
Gene editing is advancing at a faster pace than most of us can keep up with. One significant recent announcement was gene editing tool CRISPR’s application to non-genetic diseases thanks to a new ability to edit single letters in RNA.
Even as CRISPR reaches milestones like this, scientists continue to find new uses for it to treat genetic conditions. The next one that will hit clinics is a CRISPR treatment for a form of blindness called Leber congenital amaurosis (LCA).
Having been approved by the FDA in December, the treatment will be the first of its kind to be trialed in the US.
What LCA Is
LCA is a group of inherited disorders that cause severe vision loss at birth. Both parents must have a defective gene for the condition in order for a child to inherit it; 2 to 3 out of every 100,000 babies are born with LCA.
The condition can be caused by mutations in at least 14 different genes that play a role in the development of the retina (the layer of nerve cells at the back of the eye that senses light and sends signals to the brain), affecting both peripheral rod cells—which help with vision in low light—and central cone cells, which are crucial for seeing details and colors.
The pupils of people with LCA don’t react normally to light, failing to expand or contract in response to the amount of light entering the eye. For example, in one version of the disease, a mutation in the gene responsible for metabolizing vitamin A reduces the ability of photoreceptors (specialized nerve cells in the retina) to send visual information to the brain, and causes early death of photoreceptor cells.
How CRISPR Would Fix It
In CRISPR gene editing, scientists attach a synthesized sequence of guide RNA matching the target DNA sequence to the enzyme Cas-9 and introduce it into a cell’s nucleus. When the matching DNA sequence is located, Cas-9 cuts the DNA strand, and the cell then repairs the cut.
The mutations most commonly responsible for LCA occur in the CEP290, CRB1, GUCY2D, and RPE65 genes. In LCA type 10, a mutation in CEP290 causes dysfunction of a protein that helps build photoreceptor cells in the retina.
After having some of the gel-like tissue in their eyes removed, patients will have the treatment injected behind their retinas. The hope is that the patients’ DNA will repair itself in a way that restores normal protein function, ultimately fixing their photoreceptor cells and letting them see.
The treatment will be administered by Cambridge-based Editas Medicine and its Dublin-based pharmaceutical partner Allergan.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Looking Back, Looking Forward
Though this is the first study to use CRISPR to edit DNA inside the human body, it’s not the first time CRISPR-based medicine has been tested in humans, nor the first time some form of gene therapy has been used to treat LCA.
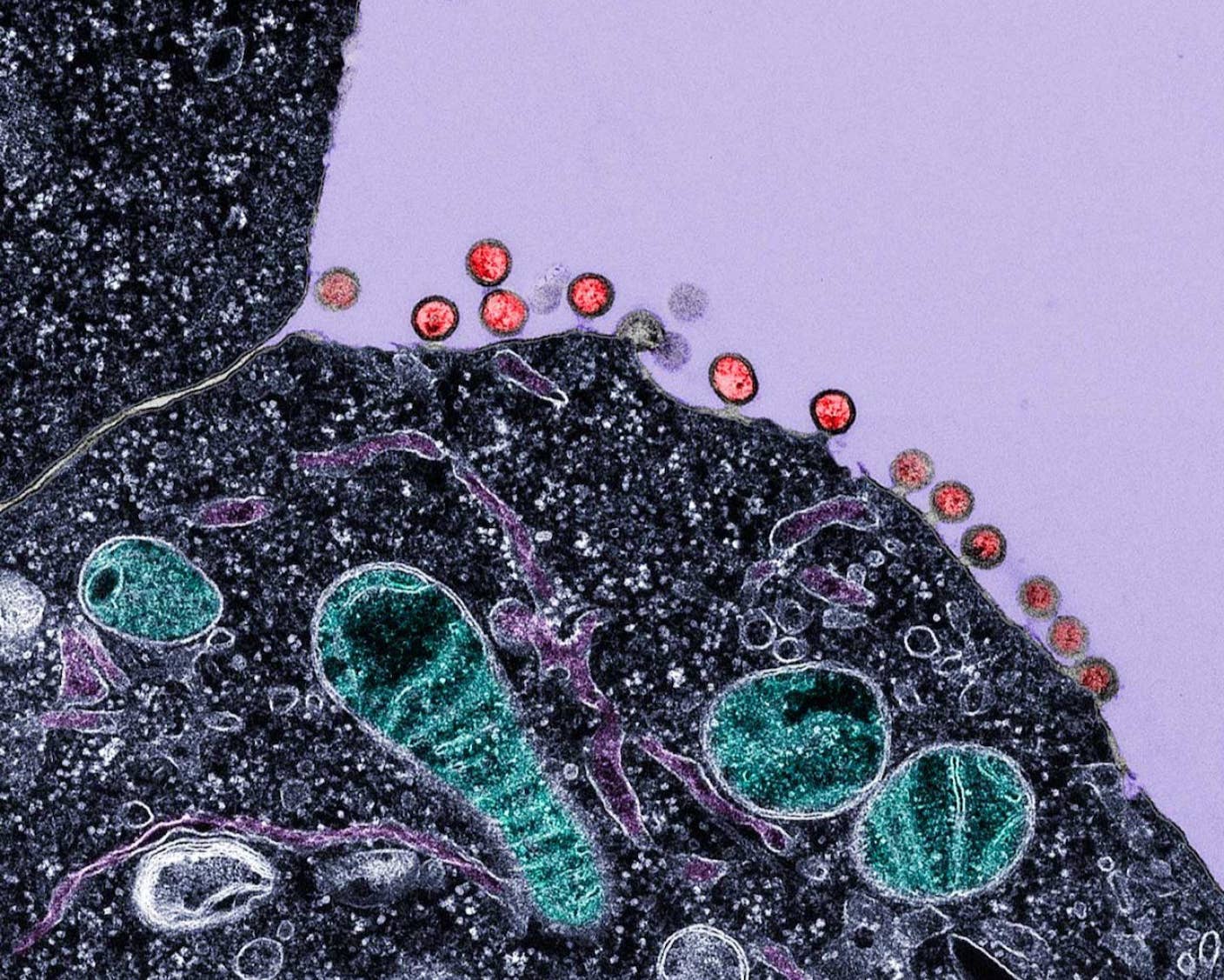
CRISPR was used to treat patients for the first time in the US earlier this year, when doctors at the University of Pennsylvania combined it with the cancer therapy CAR-T to treat two patients (the results of the treatment haven’t been released yet).
In late 2017 the FDA approved a gene therapy called Luxturna to treat LCA2, a form of the disease caused by a mutation in a different gene than that involved in type 10. It was the first directly-administered gene therapy for an inherited disease to be approved in the US. Only one other company, Sangamo Therapeutics, has tried gene editing inside the body, to treat metabolic diseases using a tool called zinc fingers.
The difference between the LCA2 treatment and the treatment that will be given to LCA10 patients is that Luxturna inserts a healthy copy of the defective gene directly into retinal cells, whereas CRISPR locates the defective gene on the DNA strand, cuts it at just the right point, and allows it to repair itself.
Though there’s no guarantee the CRISPR treatment for LCA will work, it holds a lot of promise; Luxturna successfully improved sight in its recipients with no known side effects, and a similar trial in the Netherlands produced vision improvements in about 60 percent of participants.
Treatment is slated to start this fall in 18 children and adults, and will last up to 3 years.
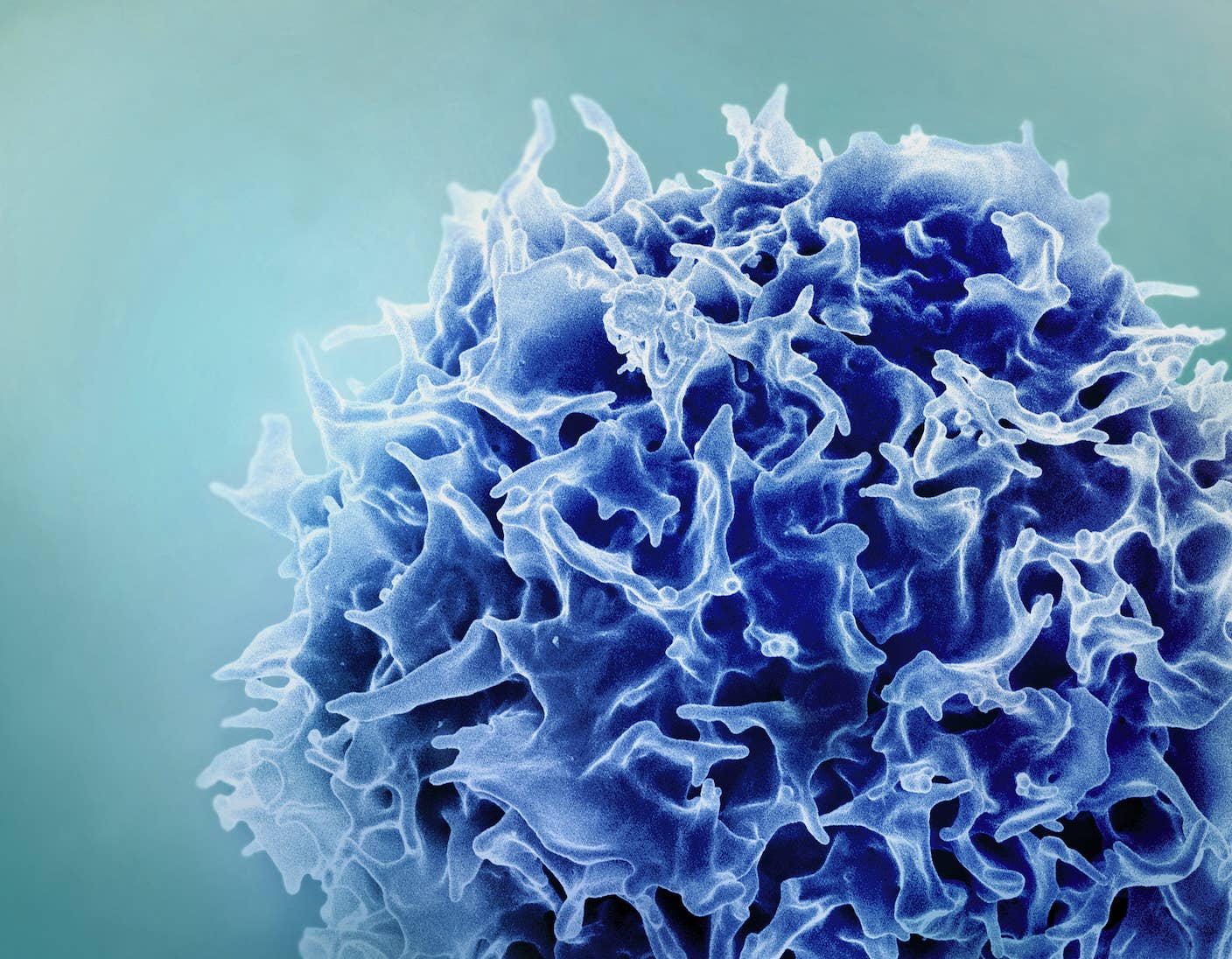
Image Credit: sie_horton / Shutterstock.com
Vanessa has been writing about science and technology for eight years and was senior editor at SingularityHub. She's interested in biotechnology and genetic engineering, the nitty-gritty of the renewable energy transition, the roles technology and science play in geopolitics and international development, and countless other topics.
Related Articles
Single Injection Transforms the Immune System Into a Cancer-Killing Machine

New Gene Drive Stops the Spread of Malaria—Without Killing Any Mosquitoes
New Immune Treatment May Suppress HIV—No Daily Pills Required
What we’re reading