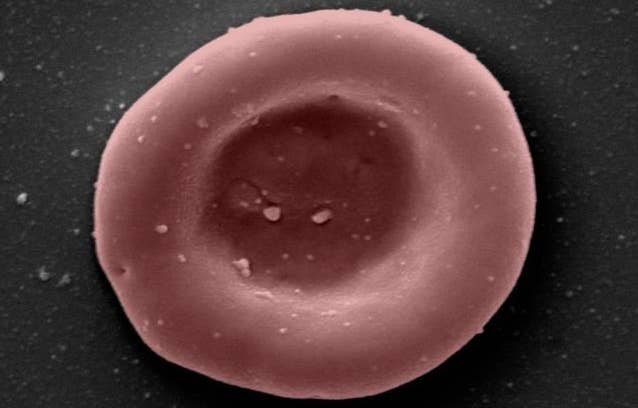
In a World First, Two People Received Transfusions of Lab-Grown Blood
Share
Of the four main blood types, the most common is Type O-positive, accounting for 37 percent of the population. Type O-negative, meanwhile, is a universal donor, meaning it carries the lowest risk of causing serious reactions for most people who receive it in a transfusion. For people with rare blood types, though, it can be near impossible to find compatible donors, making blood-related health issues far more dangerous. An initiative in the UK could present a viable solution with lab-grown blood.
For the first time ever, blood grown in a lab from adult stem cells was transfused into two people. The trial will be expanded to include 10 participants, with scientists comparing the lab-grown blood’s longevity to that of a traditional transfusion.
The infusions were part of a clinical trial spearheaded by the UK’s National Health Service Blood and Transplant (NHSBT) and the University of Bristol, and included researchers from various other UK institutions.
Decades of research went into the process that successfully grew the blood cells. Hematologists started with donated blood (from adult donors recruited through NHSBT’s donor database), and used magnetic beads to isolate and retrieve stem cells from the blood. They prodded the stem cells to differentiate into red blood cells ex vivo using a cocktail of proteins similar to those used naturally by the body.
It took three weeks for the donated blood to reach a critical mass sufficient for transfusion; a starting pool of 500,000 stem cells yielded 50 billion blood cells, and from those, 15 billion were at the right stage of development for transplantation. In this context that’s not such a huge number; the amount of transplanted blood was between 5 and 10 milliliters, or 1 to 2 teaspoons. The average healthy adult has 3.92 to 5.65 red blood cells per microliter of blood in their body.
The team’s hope is that the lab-grown blood will last longer inside recipients’ bodies than donated blood typically does. According to the BBC, since donated blood contains both young and old cells, it doesn’t tend to last more than 120 days at the most. The lab-grown blood, on the other hand, is made of all young cells, so should last longer before needing to be replaced. The team “tagged” the lab-grown cells with a radioactive substance to be able to monitor its progression in the recipients’ bloodstreams.
“If our trial, the first such in the world, is successful, it will mean that patients who currently require regular long-term blood transfusions will need fewer transfusions in future, helping transform their care,” said Cedric Ghevaert, professor in transfusion medicine and consultant hematologist the University of Cambridge and NHSBT.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


The next step is for additional participants to receive two blood transfusions spaced four months apart, one standard and one of lab-grown cells, and the results will be closely compared. No negative side effects have been observed thus far in the two people who already received transfusions.
The team envisions its technology eventually being used to make large quantities of rare blood types, which could be hugely beneficial to people with blood disorders who require frequent transfusions. Treating sickle cell anemia alone requires 250 blood donations every day (and that’s just in the UK).
“Patients who need regular or intermittent blood transfusions may [as a] result develop antibodies against minor blood groups, which makes it harder to find donor blood which can be transfused without the risk of a potentially life-threatening reaction,” said Dr. Farrukh Shah, Medical Director of Transfusion for NHS Blood and Transplant. “The need for normal blood donations to provide the vast majority of blood will remain. But the potential for this work to benefit hard to transfuse patients is very significant.”
Image Credit: NHSBT
Vanessa has been writing about science and technology for eight years and was senior editor at SingularityHub. She's interested in biotechnology and genetic engineering, the nitty-gritty of the renewable energy transition, the roles technology and science play in geopolitics and international development, and countless other topics.
Related Articles
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading