‘Breakthrough’ CRISPR Treatment Slashes Cholesterol in First Human Clinical Trial
Share
CRISPR-based therapies just hit another milestone.
In a small clinical trial with 10 people genetically prone to dangerously high levels of cholesterol, a single infusion of the precision gene editor slashed the artery-clogging fat by up to 55 percent. If all goes well, the one-shot treatment could last a lifetime.
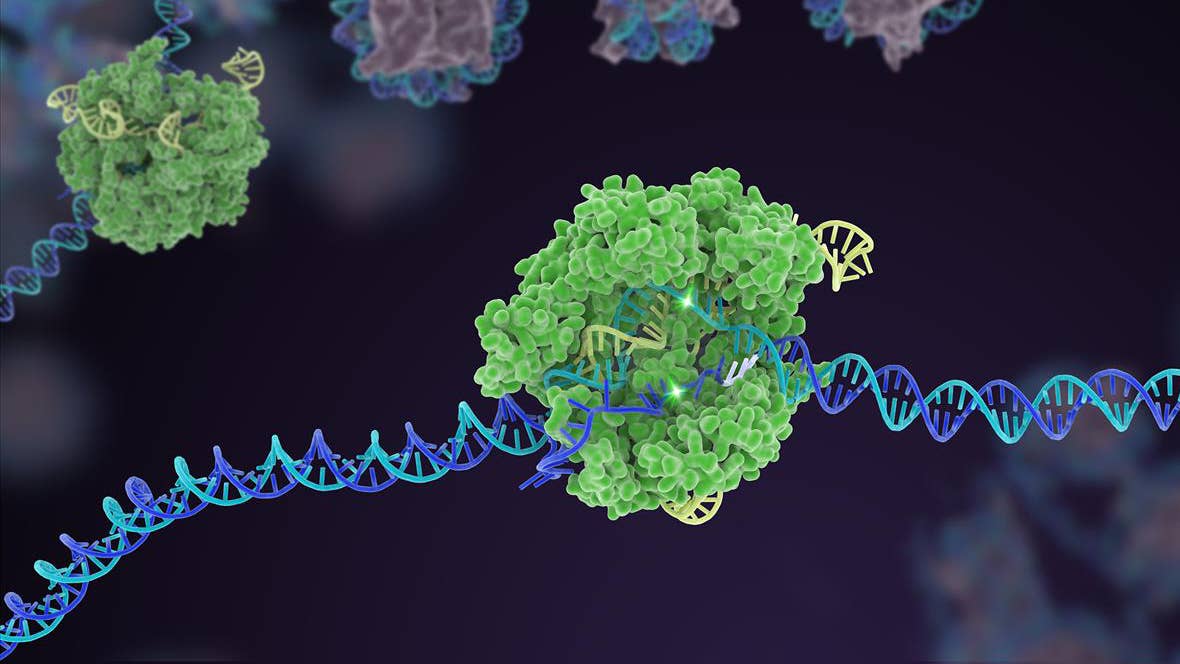
The trial, led by Verve Therapeutics, is the first to explore CRISPR for a chronic disease that’s usually managed with decades of daily pills. It also marks the first use of a newer class of gene editors directly in humans. Called base editing, the technology is more precise—and potentially safer—than the original set of CRISPR tools. The new treatment, VERVE-101, uses a base editor to disable a gene encoding a liver protein that regulates cholesterol.
To be clear, these results are just a sneak peek into the trial, which was designed to test for safety, rather than the treatment’s efficacy. Not all participants responded well. Two people suffered severe heart issues, with one case potentially related to the treatment.
Nevertheless, “it is a breakthrough to have shown in humans that in vivo [in the body] base editing works efficiently in the liver,” Dr. Gerald Schwank at the University of Zurich, who wasn’t involved in the trial, told Science.
Give Your Heart a Break
CRISPR has worked wonders for previously untreatable cancers. Last week, it was also approved in the United Kingdom for the blood diseases sickle cell and beta thalassemia.
For these treatments, scientists extract immune cells or blood cells from the body, edit the cells using CRISPR to correct the genetic mistake, and reinfuse the treated cells into the patient. For edited cells to “take,” patients must undergo a grueling treatment to wipe out existing diseased cells in the bone marrow and open space for the edited replacements.
Verve is taking a different approach: Instead of isolating cells for gene editing, the tools are infused into the bloodstream where they edit genes directly inside the body. It’s a big gamble. Most of our cells contain the same DNA. Once injected, the tools could go on a rampage and edit the targeted gene throughout the body, causing dangerous side effects.
Verve tackled this concern head on by pairing base editing with nanoparticles.
The trial targeted PCSK9, a liver protein that keeps low-density lipoprotein (LDL), or “bad cholesterol,” levels at bay. In familial hypercholesterolemia, a single mutated letter in PCSK9 alters its function, causing LDL levels to grow dangerously. People with this inherited disorder are at risk of life-threatening heart problems by the age of 50 and need to take statin drugs to keep their cholesterol in check. But the lifelong regime is tough to maintain.
A Targeted CRISPR Torpedo
Verve designed a “one-and-done” treatment to correct the PCSK9 mutation in these patients.
The therapy employs two key strategies to boost efficacy.
The first is called base editing. The original CRISPR toolset acts like scissors, cutting both strands of DNA, making the edit, and patching the ends back together. The process often leaves room for mistakes, such as the unintended rearranging of sequences that could turn on cancer genes, leading some experts to call it “genetic vandalism.” Base editing, in contrast, is far more precise. Like a scalpel, base editors only nick one DNA strand, and are therefore far less likely to injure non-targeted parts of the genome.
Verve’s treatment encodes the base editor in two different RNA molecules. One instructs the cells to make the components of the gene editing tool—similar to how Covid-19 vaccines work. The other strand of RNA guides the tool to PCSK9. Once edited, the treated gene produces a shortened, non-functional version of the faulty protein responsible for the condition.
The delivery method also boosts efficacy. Base editing components can be encoded into harmless viruses or wrapped inside fatty nanoparticles for delivery. Verve took the second approach because these nanoparticles are often first shuttled into the liver—exactly where the treatment should go—and are less likely to cause an immune reaction than viruses.
There’s just one problem. Base editing has never been used to edit genes in the body before.
A non-human trial in 2021 showed the idea could work. In macaque monkeys, a single shot of the editor into the bloodstream reduced the gene’s function in the liver, causing LDL levels to drop 60 percent. The treatment lasted at least eight months with barely any side effects.
Safety First
The new trial built on previous results to assess the treatment’s safety in 10 patients with familial hypercholesterolemia. One patient dropped out before completing the trial.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


The team was careful. To detect potential side effects, six patients were treated with a small dose unlikely to reverse the disorder.
Three patients received a higher dose of the base editor and saw dramatic effects. PCSK9 protein levels in their livers dropped between 47 and 84 percent. Circulating LDL fell to about half its prior levels—an effect that lasted at least six months. Follow-ups are ongoing.
The efficacy of the higher dose came at a price. At lower doses, the treatment was well tolerated overall with minimal side effects. But at higher doses, it seemed to temporarily tax the liver, bumping up markers for liver stress that gradually subsided.
More troubling were two severe events in patients with advanced heart blockage. One person receiving a low dose died from cardiac arrest about five weeks after the treatment. According to a review board, the death was likely due to underlying conditions, not the treatment.
Another patient infused with a higher dose suffered a heart attack a day after treatment, suggesting the episode could have been related. However, he had intermittent chest pains before the infusion that hadn’t been disclosed to the team. His symptoms would have excluded him from the trial.
A Promising Path
Overall, an independent board monitoring data and safety determined the treatment safe. Still, there are plenty of unknowns. Like other gene editing tools, base editing poses the risk of off-target snips—something this trial did not specifically examine. Long-term safety and efficacy of the treatment are also unknown.
But the team is encouraged by these early results. “We are excited to have reached this milestone of positive first-in-human data supporting the significant potential for in vivo liver gene editing as a treatment for patients with [familial hypercholesterolemia],” said Dr. Sekar Kathiresan, CEO and cofounder of Verve.
The trial was conducted in the United Kingdom and New Zealand. Recently, US regulators approved the therapy for testing. They plan to enroll roughly 40 more patients.
Meanwhile, a new version of the therapy, VERVE-102, is already in the works. The newcomer uses a similar base editing technology and an upgraded nanoparticle carrier with potentially better targeting.
If all goes well, the team will launch a randomized, placebo-controlled trial by 2025. So far, the company hasn’t released a price tag for the therapy. But the cost of existing gene therapies can run into the millions of dollars.
To Kathiresan, treatments like this one could benefit more than patients with familial hypercholesterolemia. High cholesterol is a leading health problem. A dose of the base editor in middle age could potentially nip cholesterol buildup in the bud—and in turn, lower risk of heart disease and death.
“That’s the ultimate vision,” he said.
Image Credit: Scientific Animations / Wikimedia Commons
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading