The Legally Blind See Again With an Implant the Size of a Grain of Salt

Share
Seeing is believing. Our perception of the world heavily relies on vision.
What we see depends on cells in the retina, which sit behind the eyes. These delicate cells transform light into electrical pulses that go to the brain for further processing.
But because of age, disease, or genetics, retinal cells often break down. For people with geographic atrophy—a disease which gradually destroys retinal cells—their eyes struggle to focus on text, recognize faces, and decipher color or textures in the dark. The disease especially attacks central vision, which lets our eyes focus on specific things.
The result is seeing the world through a blurry lens. Walking down the street in dim light becomes a nightmare, each surface looking like a distorted version of itself. Reading a book or watching a movie is more frustrating than relaxing.
But the retina is hard to regenerate, and the number of transplant donors can’t meet demand. A small clinical trial may have a solution. Led by Science Corporation, a brain-machine interface company headquartered in Alameda, California, the study implanted a tiny chip that acts like a replacement retina in 38 participants who were legally blind.
Dubbed the PRIMAvera trial, the volunteers wore custom-designed eyewear with a camera acting as a “digital eye.” Captured images were then transmitted to the implanted artificial retina, which translated the information into electrical signals for the brain to decipher.
Preliminary results found a boost in the participants’ ability to read the eye exam scale—a common test of random letters, with each line smaller than the last. Some could even read longer texts in a dim environment at home with the camera’s “zoom-and-enhance” function.
The trial is ongoing, with final results expected in 2026—three years after the implant. But according to Frank Holz at the University of Bonn Ernst-Abbe-Strasse in Germany, the study’s scientific coordinator, the results are a “milestone” for geographic atrophy resulting from age.
“Prior to this, there have been no real treatment options for these patients,” he said in a press release.
Max Hodak, CEO of Science Corp and former president of Elon Musk’s Neuralink, said, “To my knowledge, this is the first time that restoration of the ability to fluently read has ever been definitively shown in blind patients.”
Eyes Wide Open
The eye is a biological wonder. The eyeball’s layers act as a lens focusing light onto the retina—the eye’s visual “sensor.” The retina contains two types of light-sensitive cells: Rods and cones.
The rods mostly line the outer edges of the retina, letting us see shapes and shadows in the dark or at the periphery. But these cells can’t detect color or sharpen their focus, which is why night vision feels blurrier. However, rods readily pick up action at the edges of sight—such as seeing rapidly moving things out of the corner of your eye.
Cones pick up the slack. These cells are mostly in the center of the retina and can detect vibrant colors and sharply focus on specific things, like the words you’re currently reading.
Both cell types rely on other cells to flourish. These cells coat the retina, and like soil in a garden, provide a solid foundation in which the rods and cones can grow.
With age, all these cells gradually deteriorate, sometimes resulting in age-related macular degeneration and the gradual loss of central vision. It’s a common condition that affects nearly 20 million Americans aged 40 or older. Details become hard to see; straight lines may seem crooked; colors look dim, especially in low-light conditions. Later stages, called geographic atrophy, result in legal blindness.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Scientists have long searched for a treatment. One idea is to use a 3D-printed stem cell patch made out of the base “garden soil” cells that support light-sensitive rods and cones. Here, doctors transform a patient’s own blood cells into healthy retinal support cells, attach them to a biodegradable scaffold, and transplant them into the eye.
Initial results showed the patch integrated into the retina and slowed and even reversed the disease. But this can take six months and is tailored for each patient, making it difficult to scale.
A New Vision
The Prima system eschews regeneration for a wireless microchip that replaces parts of the retina. The two-millimeter square implant—roughly the size of a grain of salt—is surgically inserted under the retina. The procedure may sound daunting, but according to Wired, it takes only 80 minutes, less time than your average movie. Each chip contains nearly 400 light-sensitive pixels, which convert light patterns into electrical pulses the brain can interpret. The system also includes a pair of glasses with a camera to capture visual information and beam it to the chip using infrared light.
Together, the components work like our eyes do: Images from the camera are sent to the artificial retina “chip,” which transform them into electrical signals for the brain.
Initial results were promising. According to the company, the patients had improved visual acuity a year after the implant. At the beginning of the study, most were considered legally blind with an average vision of 20/450, compared to the normal 20/20. When challenged with an eye exam test, the patients could read, on average, roughly 23 more letters—or five more lines down the chart—compared to tests taken before they received the implant. One patient especially excelled, improving their performance by 59 letters—over 11 lines.
The Prima implant also impacted their daily lives. Participants were able to read, play cards, and tackle crossword puzzles—all activities that require central vision.
While impressive, the system didn’t work for everyone. The implant caused serious side effects in some participants—such as a small tear in the retina—which were mostly resolved according to the company. Some people also experienced blood leaks under the retina that were promptly treated. However, few details regarding the injuries or treatments were released.
The trial is ongoing, with the goal of following participants for three years to track improvements and monitor side effects. The team is also looking to measure their quality of life—how the system affects daily activities that require vision and mental health.
The trial “represents an enormous turning point for the field, and we’re incredibly excited to bring this important technology to market over the next few years,” said Hodak.
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
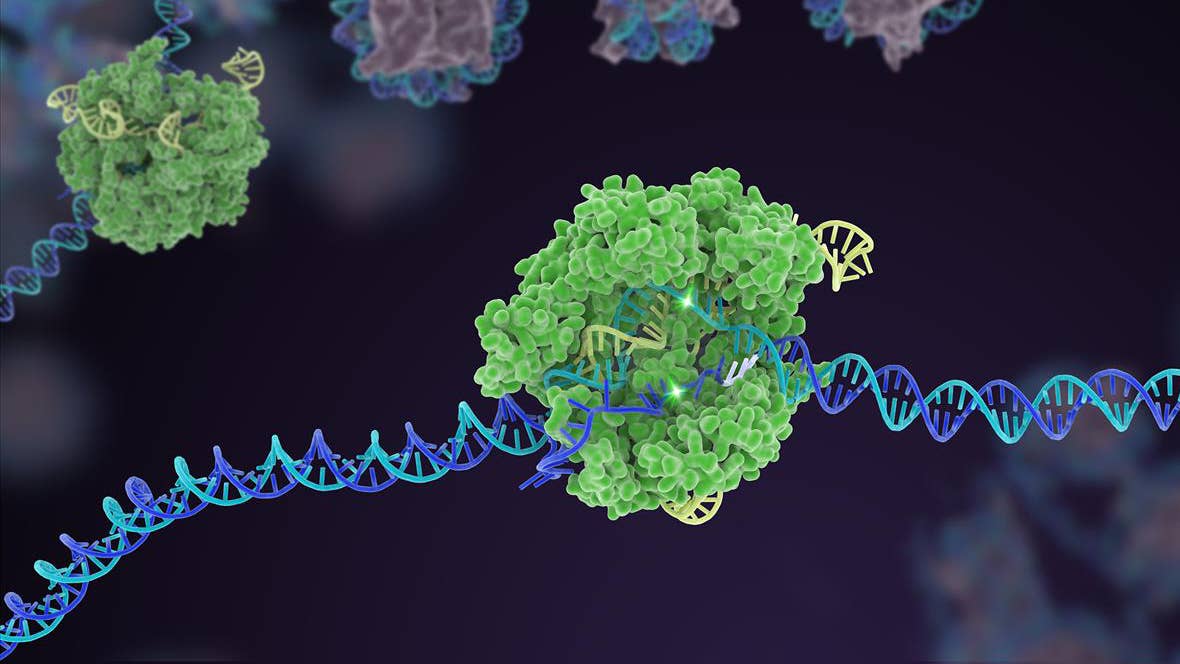
Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading