Scientists Just Transplanted a Pig Liver Into a Person for the First Time
The liver performed basic functions but isn’t yet a full replacement.

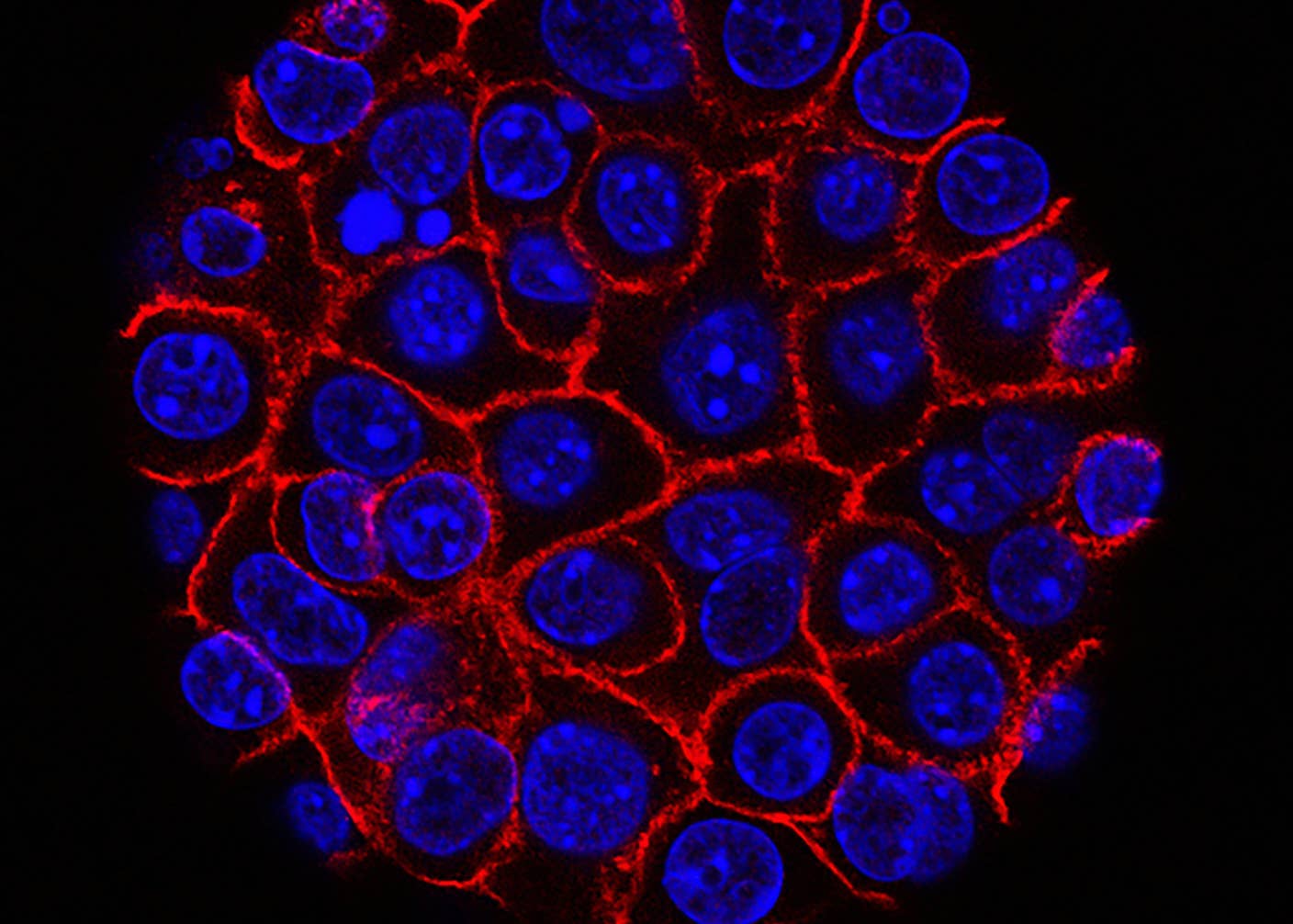
Image Credit
Kenneth Schipper on Unsplash
Share
Our liver has admirable regenerative properties. But it takes a beating every day. Eventually, its tissues scar, and if the organ fails, a liver transplant is the only solution.
Donor livers are hard to come by, however. This week, a Chinese team turned to another source—pig livers—and published the first results showing how they function inside a human recipient. The liver in the study underwent heavy gene editing to rid it of genes that trigger immune rejection and add genes making it appear more human to the body.
Just two hours after transplant, the pig liver began producing bile, a type of digestive fluid that breaks down fat. The organ remained functional until the end of the experiment 10 days later, without marked signs of rejection or inflammation.
“This is the first time we tried to unravel whether the pig liver could work well in the human body,” said study author Lin Wang at Xijing Hospital in China in a press briefing. The pig liver is meant to be a stop-gap measure rather than a full replacement. It could temporarily keep patients alive until a human donor organ becomes available or the patient’s own liver recovers.
“The study represents a milestone in the history of liver xenotransplantation,” said Iván Fernández Vega at the University of Oviedo in Spain, who was not involved in the study. “I found the work very relevant, but we have to be cautious.”
Crossing Species
There’s a severe lack of donated organs. As of March 2025, over 104,600 people are on a transplant waitlist, which could take months, if not years. Some don’t survive the wait.
Xenotransplantation, or the transplantation of organs from one animal into another, offers another solution. For the past decade, scientists have been eyeing other species as resources for functional organs that could replace broken human body parts. Bama miniaturized pigs are especially promising because their internal organs are similar in size and function to ours.
But there are caveats. Pig organs are dotted with sugars that spur our immune systems into action. Immune cells attack the foreign organ, damaging its function or triggering rejection.
There’s also the risk posed by porcine endogenous retroviruses or PERVs. These are tricky viruses embedded inside the genomes of all pigs. Although they don’t seem to harm pigs, they can infect some human cells and potentially lead to disease.
Xenotransplant efforts over the past decade have tried gene editing pig organs to rid them of PERVs. Other edits inhibit genes responsible for immune rejection and make the organs appear more human to the body.
There have been successes. Genetically engineered pig hearts transplanted into baboons with heart failure allowed them to thrive for over six months. Pig kidney grafts with 69 genetic edits retained function after transplantation in monkeys.
And although highly experimental, xenotransplantation has already been used in humans. In 2021, a team performed the first transplant of a genetically modified pig kidney into a brain-dead person. The kidney was attached to blood vessels in the upper leg outside the belly and covered with a protective shield.
Since then, surgeons have transplanted hearts, kidneys, and a thymus directly inside the bodies of living volunteers, with mixed results. One pig heart recipient soon passed away after the xenotransplant. Another fared better with a pig kidney: The 53-year-old grandma returned home this February after receiving the organ late last year.
Her ”recovery from a long history of kidney failure and dialysis treatment has been nothing short of remarkable,” said study lead Robert Montgomery at NYU Langone Transplant Institute at the time.
Liver xenotransplants, however, pose additional problems.
The organ “is so complicated,” said Wang. As the ultimate multitasker, it metabolizes drugs and other chemicals, makes bile and other digestive juices, cleans out old blood cells, and produces proteins for blood clotting. Each of these functions is orchestrated by a symphony of molecules that could differ between pigs and humans. A mismatch could result in a pig liver that can’t work in the human body or one that triggers dangerous immune responses.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


In 2023, a team from the University of Pennsylvania took a stab at the problem. They connected a genetically engineered pig liver to the bloodstream of a brain-dead person with the organ outside the body. The donor liver, engineered by the biotechnology company eGenesis to reduce the chance of immune rejection, remained healthy for at least 72 hours.
Plus One
The new study aimed to show that a pig liver transplant could last longer and perform its usual tasks. The team sourced the liver from Clonorgan Biotechnology based in Chengdu, China.
The donor organ was from a seven-month-old Bama miniature pig and had six gene edits. The majority of the edits were designed to prevent hyperacute rejection, where the immune system launches a full onslaught against the transplant within minutes.
The recipient was a brain-dead, middle-aged man who still had a working liver. Rather than trying to replace his liver, the team wanted to find out whether a pig liver could survive and function inside a human body while performing its normal roles.
Surgeons hooked the gene-edited pig liver to the donor’s blood supply and monitored it for 10 days—the amount of time the recipient’s family approved for the experiment. Within hours, the organ began synthesizing and pumping out bile at a gradually increasing volume. The liver also made albumin, a protein crucial for maintaining fluids and transporting molecules.
Blood from the recipient flowed smoothly throughout the liver, which likely prevented blood clots often associated with liver transplants. Thanks to immunosuppressant drugs, the patient’s immune system stayed relatively quiet and didn’t attack the pig organ.
“This is the world’s first [published] case of a transplant of a genetically modified pig liver into a brain-dead human,” said Rafael Matesanz, creator and founder of the National Transplant Organization in Spain, who was not involved in the work.
Many questions remain. The liver has multiple functions, but the study only tested bile and albumin production. Could the pig liver also filter toxins from the blood or break down medications? Also, the study only observed one person for a relatively short time. The results might not hold for other demographics, and the transplant could falter down the road.
And because the volunteer still had a functional liver, “we cannot extrapolate the extent to which this xenograft would have supported a patient in liver failure,” said Peter Friend at the University of Oxford, who was not involved in the study.
Even so, a temporary bridge transplant—where a pig liver would support bodily functions short-term while the recipient waits for a permanent transplant—could save lives.
The same team recently completed a full pig-to-human liver transplant, swapping out the liver of a brain-dead human with one from a genetically-modified pig. They plan to release the data in a future publication. “Whether it could replace the original human liver in the future [is unknown],” said Wang at the press briefing. “It is our dream to make this achievement.”
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles
These Supercharged Immune Cells Completely Eliminated Solid Tumors in Mice

Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought
What we’re reading