Diabetes Defeated by a Microchip? Silicon Pancreas Hits Trials
Share
Most people who treat their Type I Diabetes must still rely on pricking their finger and testing their blood several times everyday. Researchers at the Imperial College London want to give that job to a microchip. Pantelis Georgiou and Nick Oliver at ICL have developed a special blood glucose control chip that reacts to changes in sugar levels just like the cells in your body. The 'Silicon Pancreas' mimics the insulin controlling beta cells, as well as the glucagon controlling alpha cells, normally found in the healthy organ. In diabetics, beta cells are destroyed by the body's immune system and alpha cells tend to suffer over the long term. When paired with a continuous glucose monitor embedded on the skin, and a pair of insulin and glucagon pumps, the Silicon Pancreas should be able to give diabetics an approximate response to blood sugar levels close to what their bodies would normally produce. According to IEEE Spectrum, Georgiou and Oliver will be working with colleagues in two London hospitals to begin trials with the Silicon Pancreas for 10 patients in 2011. You can watch their short explanation of the technology in the video below. If successful, this program could be expanded to many more patients, and it may prove that a cybernetic fix could be a viable solution for diabetes.
Of course, there have been other teams attempting to turn diabetics into cyborgs. Recently we discussed a device developed with help from the US Juvenile Diabetes Research Foundation that closely resembles the Silicon Pancreas in function. The JDRF device uses a continuous blood glucose monitor, an insulin (and glucagon) pump, and a wearable controlling computer to provide a diabetes patient with the correct hormones in their blood 24 hours a day. That solution had several successes in 2010, including a 17 person trial reported in The Lancet that showed it was equal to or better than standard manual testing and treatment performed by diabetics. What sets the Imperial Colege London Silicon Pancreas apart from the JRDF device, however, is the microchip it uses. As Georgiou and Oliver explain below, that chip is closely mimicking the response of cells in your body.
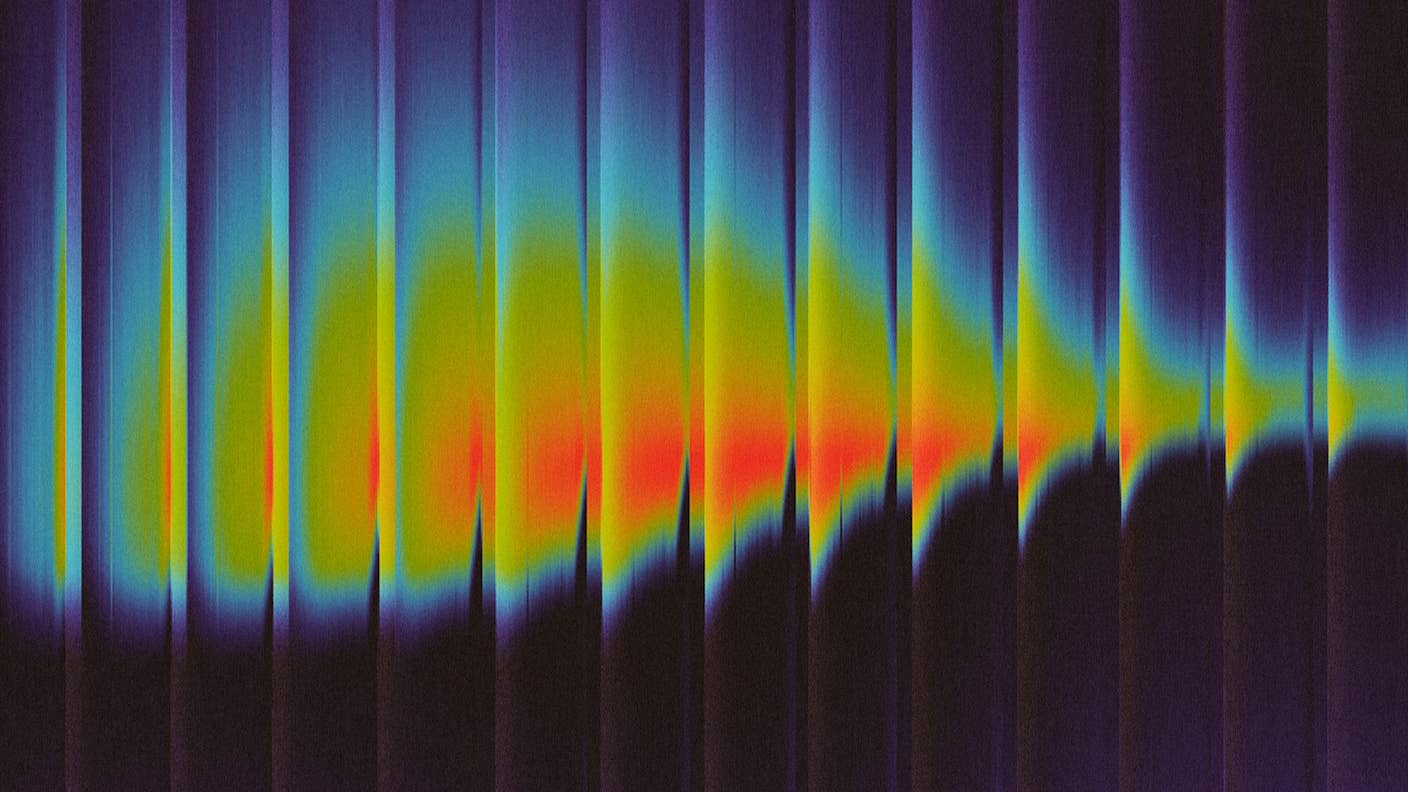
Alpha cells and beta cells in the pancreas respond differently to blood sugar levels. When glucose is high, beta cells are stimulated to release insulin in large spikes that can be plateaued as needed. After a spike, beta cells tend to remain silent for longer periods of time. Alpha cells, in contrast, release glucagon when blood sugar levels are low, and they do so in rapid bursts. The frequency of these bursts changes as glucose levels rise and fall.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


ICL's Silicon Pancreas has two sets of control algorithm built into it that copy these types of alpha and beta cell responses. When the virtual cells are triggered (via the blood sugar monitor readings) the chip activates the appropriate insulin or glucagon pump in the same way that the real cells would release those hormones. In contrast, the JRDF device has control software that monitors levels and predicts where they may be in the future, releasing insulin or glucose as needed. The first is a behavioral technique, the second a predictive one.
Clearly, with the ICL trial yet to have been completed, it's too soon to know which approach will prove to be superior. Should we be trying to replicate the body's response or planning a better structure of our own? The answer is probably 'yes' to both. Complex diseases typically require complex engineering solutions and there may be some optimum combination of the two approaches that will best serve diabetics. Or maybe one approach will simply work better. Even then, we'll need to research both techniques in order to find out. ...Yeah, I'm pretty much always in favor of more research.
We should keep in mind, however, that no matter which control paradigm (or combination of paradigms) we adopt, current cybernetic solutions have their limitations. Especially in response times. Georgiou and Oliver are using a blood glucose monitor situated in the skin. The JRDF device measures glucose in the interstitial fluid. Neither of these is going to be as fast or accurate as a device embedded in the blood, and insulin pumps have finite reactions speeds as well. Perhaps one day we'll have artificial pancreases that are completely internal and overcome these limitations, but that's years ahead of us still.
And even though implants like the JRDF device and the Silicon Pancreas have the potential to defeat diabetes by letting us control our blood sugar levels, neither is going to be a true cure. For that we will need to deal with the actual problem - the body's loss of healthy beta cells. As we've discussed before, that's probably going to come through stem cell therapies, some of which are already having great success. Cybernetic solutions for the disease are remarkable, and growing nearer to use, but they are likely only a stepping stone towards even better treatments. In the future, we won't simply defeat diabetes, we'll remove it from our bodies entirely. At least, I hope so.
[image credit: Pantelis Georgiou via IEEE Spectrum]
[video credits: Imperial College London]
[sources: Imperial College London, IEEE Spectrum]
Related Articles

AI-Designed Antibodies Are Racing Toward Clinical Trials

Sci-Fi Cloaking Technology Takes a Step Closer to Reality With Synthetic Skin Like an Octopus
This Week’s Awesome Tech Stories From Around the Web (Through January 10)
What we’re reading