As Safer Fetal Genetic Tests Arrive, Abortions Could Rise

Share
The impending arrival of non-invasive prenatal diagnosis (NIPD) will allow more parents than ever before to discover congenital disorders early in pregnancy...but will it also lead to an increase in abortions? Because of the risks associated with older methods, very few fetuses actually undergo rigorous screening in today's clinic. The broadening scope of prenatal diagnosis has prompted speculation about rising abortion rates, and merged with a growing understanding of the human genome, some predict that early genotyping could open the door to eugenics through selecting babies based on prenatally determined traits. However, the complex interplay with sociocultural forces and parallel trends in reproductive technology will make abortion rates exceedingly difficult to forecast over the long term. Overall, the immediate benefits of NIPD will far outweigh the risks, and it could prove to be an invaluable asset for physicians and families.
To appreciate the advances in NIPD, it’s necessary to understand the dire status of prenatal diagnosis. Before pregnancies undergo invasive testing, many mothers are screened using a non-invasive blood test that looks for biomarkers linked to certain congenital disorders. However, these tests are not very accurate, and invasive methods are still required if the results are positive. There are also other risk factors, such as age, that determine if the pregnancy qualifies for further testing. Unfortunately, these tests (amniocentesis or CVS) carry a troubling risk of miscarriage. The risks even apply to healthy fetuses who receive a false-positive on the blood screen. Therefore, many accidental miscarriages occur in which no disorder is detected. Using traditional methods, the prenatal diagnosis process is emotionally brutal for future parents. It’s clear that a safe and accurate test is needed.

A Down syndrome study that illustrates the status quo of prenatal screening. Pregnancies in Wales and England were screened using initial biomarker testing, followed by amniocentesis or CVS to confirm or reject the diagnosis. The false positives for the initial blood screen are huge!
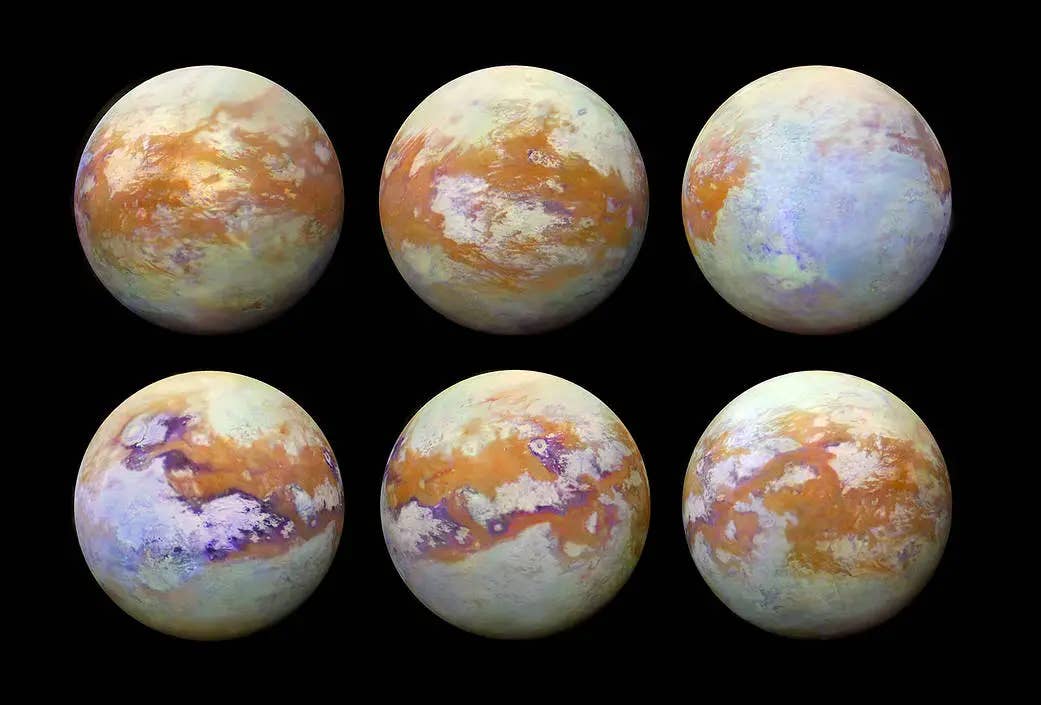
New developments in sequencing technology show promise. Dennis Lo of the Chinese University of Hong Kong has spent years finding the billion little bits of fetal DNA in maternal blood and reconstructing them. Recent results demonstrated that the maternal and fetal genomes co-existed at a relative proportion to each other in the mother's blood, allowing his lab to quantify imbalances. Therefore, an over-representation of mutations in maternal blood would indicate the presence of a genetic disorder in the fetus.
In a recent BMJ article, his team tested the feasibility of NIPD for Down syndrome on a large scale. After refining their sequencing protocol, they were able to detect trisomy-21 (Down Syndrome) with a predictive accuracy of 96.6%. Dr. Lo's lab also applied the “genetic imbalance” approach to hemophilia, a blood clotting disorder. In results to be published in an upcoming issue of Blood, the team recruited seven pregnant women who were carriers of genes known to cause hemophilia. Using only 10 milliliter blood samples, they accurately detected hemophilia in four pregnancies due to an abnormally high presence of the mutant gene. It's important to note that for both studies, the pregnancies were already considered “high-risk” because of age or genetic background of the parents, so the accuracy of this test in general population is yet to be determined. However, once NIPD reaches the doctor's office, there will be several immediate benefits. Currently, few mothers-to-be opt for screening due to the hazards. Accurate NIPD will take that risk out of the equation, allowing accurate prenatal screening to become standard care. Moreover, it will inform the decisions of physicians, who could tweak their neonatal protocol if they know the child has hemophilia or disorders that complicate the birth process. Of course, the greatest benefit will be that no parent will have to endure an accidental miscarriage because of a test.

Dr. Lo's non-invasive technique for diagnosing hemophilia. Each square represents a well. Red - Mutant Gene Detected, Blue - Normal Gene Detected. If the proportion of mutant-positive wells was significantly high, then the subject was classified as a hemophiliac (see graph).
The Dawn of Prenatal Eugenics?
Now that we know the positives of accurate NIPD, it’s time to talk about the elephant in the room: the possibility of rising abortion rates. In a Nature op-ed, Henry T. Greely points out the shift of sex ratios in Asia after the introduction of accessible, inexpensive ultrasound. One study found a 759:1000 girl to boy ratio. After noting that these differences were not caused by still birth, they concluded that “selective abortion of female fetuses [was] the most plausible explanation.” Because of this disturbing phenomenon, Greely wonders if prenatal genotyping could also encourage prenatal selection. In the article, he makes a dire prediction:
Fears of eugenics will increase as such testing moves from fatal diseases to less serious medical conditions and then on to nonmedical characteristics — sex selection today; skin, hair and eye colour tomorrow; perhaps, eventually, traits such as some cognitive or physical abilities.
Is NIPD really a sign of reproductive dystopia? For those worried about high abortion rates for birth defects, you may be surprised that this is already a reality. The table below summarizes studies from Singapore to the U.S. that looked at abortions following the diagnosis of a variety of congenital disorders.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.



According to this meta-analysis, an overwhelming majority of pregnancies in which Down Syndrome was detected resulted in an abortion (1980s: 96%, 1990s: 92%). For other congenital disorders, the rates of termination were similarly high for both decades.
Evidently, most high-risk pregnancies in 1980s and 1990s studies ended with an abortion if serious congenital dysfunction was detected. If NIPD expands accurate testing to all pregnancies, will we see a rise in abortions? Provided that termination rates remain high for birth defects, then most likely, but the increase will be difficult to forecast. The current U.S. abortion rate is around 2 per 100 women of child-bearing age, and the prevalence of live-births with congenital disorders is about 1 out of 100 pregnancies. Assuming that all fetuses with congenital disorders are aborted (a highly improbable scenario), then the annual abortions would jump about 50%. However, any increase would face the overarching trend of falling abortion rates. While preimplantation genetic diagnosis (PGD) could be contributing to this decline, there were only 500 PGD babies born in the 1990s, a negligible proportion of all abortions given in that decade. Also, rates of termination after prenatal diagnosis have decreased to a greater extent in the American southeast, home of the Bible Belt. Although this is correlational, it suggests that cultural values could be a significant driver of parental decisions and technology is not the only determinant. These variables ensure that accurately predicting abortion trends will be difficult, if not impossible. Regardless of the final outcome, abortions will continue to be unacceptable under any circumstances for some. However, one should keep in mind that NIPD will save the pregnancies that would have been accidentally cut short by invasive methods. At least the greatly diminished threat of miscarriage will give more parents the opportunity to decide.
How about prenatal genotyping of nonmedical conditions? Will many parents intentionally terminate a pregnancy if they find the potential intelligence, strength, or eye color of the fetus to be undesirable? Not yet. Genes are the template, not the final product. It’s now known that epigenetic factors (modifications of DNA expression patterns) play a significant role in who we become. Also, the brain has proven repeatedly that it can adapt to even the most profound deficits. For example, who would have thought that a girl born with half a brain could sustain a reasonable quality of life? If complex genotyping is ever common, it will be important for genetic counselors to educate parents on how neuroplasticity and epigenetics can help children live beyond their genes. Nonetheless, even with a concerted effort from counselors, some parents would end a pregnancy over trivial characteristics.
Another factor to consider is that complex genetics is still in the early stages, and other technologies developing in the background could alter the eugenics fears. Why abort a pregnancy when you can use in utero gene therapy? Why even conceive of a child with a disorder if advanced pre-conception testing and karyomapping is available? These technologies come with their own ethical baggage, but that’s another fight for another day.
Few issues can ignite dystopian discourse like reproductive science. However, I hope we can collectively revel in the progress made in NIPD. No more scary needles for amniocentesis. No more risks of losing a child over a test result. Ethical concerns will always be a part of science and medicine, and no one really knows if technology will take us to unprecedented heights or lead us to our downfall. However, I know that, for the foreseeable future, NIPD will be a damn good thing.
[Image Credits: Wylio, Down Syndrome Research and Practice (modified), Blood, Prenatal Diagnosis]
[Sources: BMJ, Blood, Nature Publishing]
Related Articles
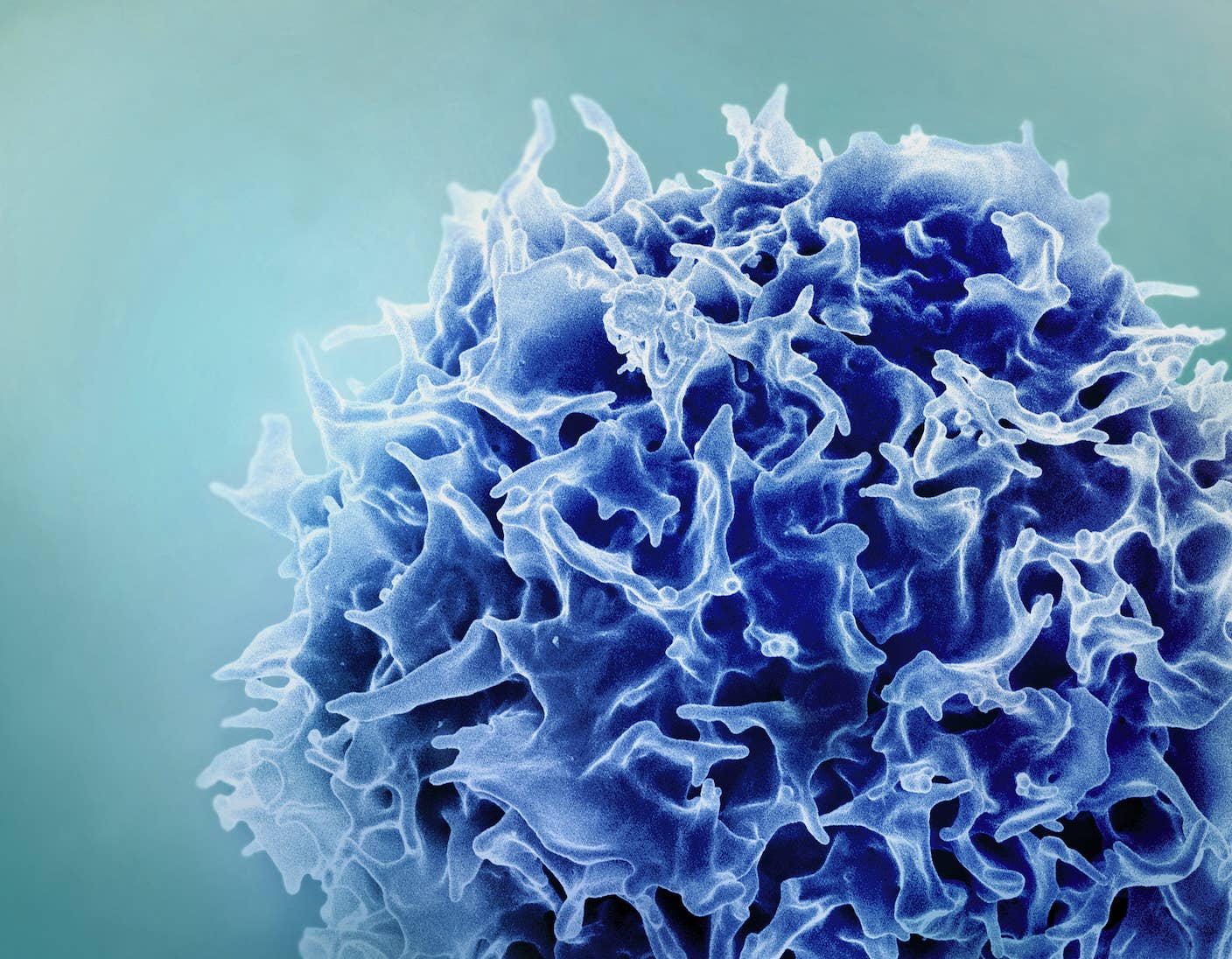
Single Injection Transforms the Immune System Into a Cancer-Killing Machine
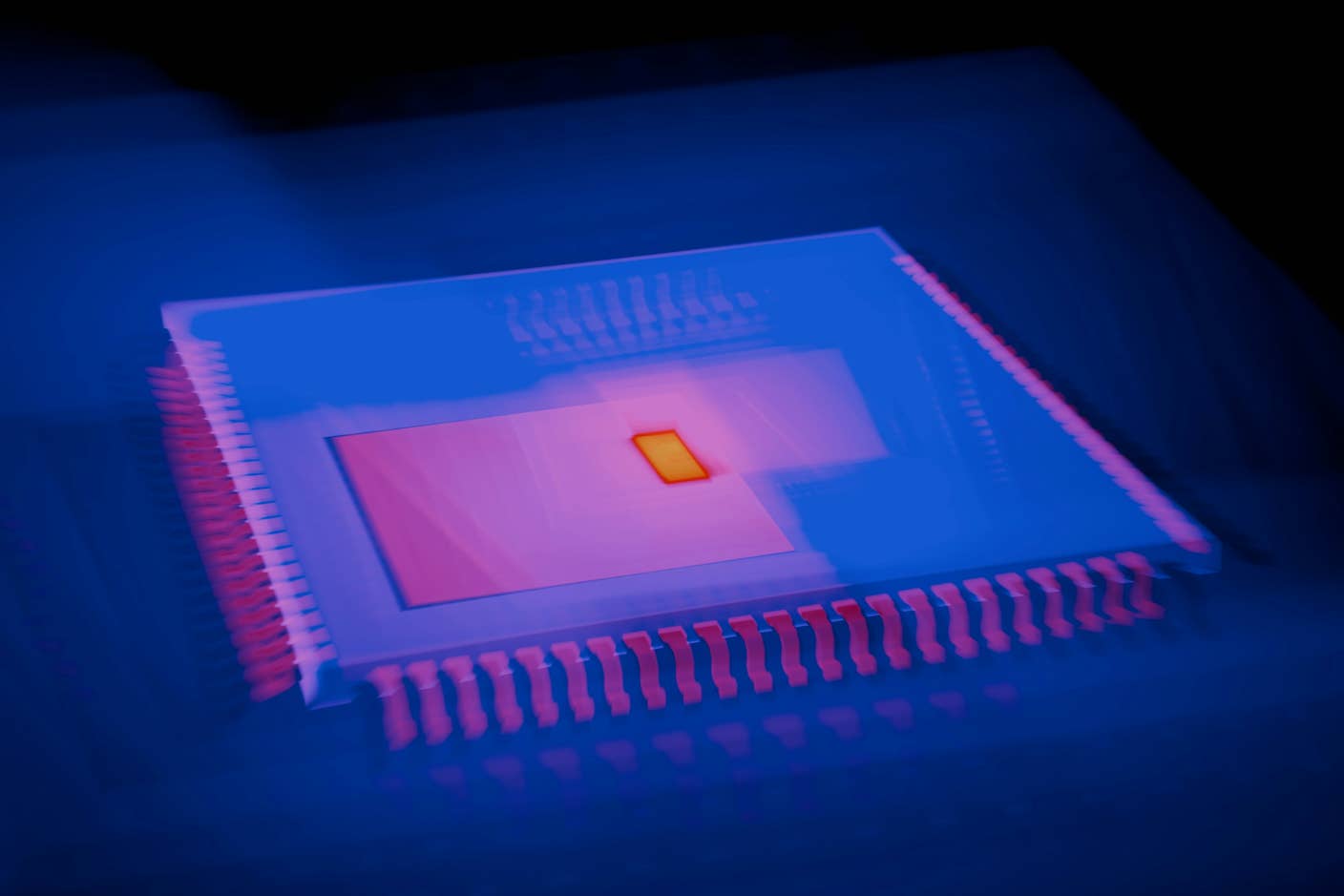
This Light-Powered AI Chip Is 100x Faster Than a Top Nvidia GPU
This Week’s Awesome Tech Stories From Around the Web (Through December 20)
What we’re reading