The Food and Drug Administration has just approved a device that is integrated into pills and let’s doctors know when patients take their medicine – and when they don’t. Adherence to prescriptions is a serious problem, as about half of all patients don’t take medications the way they’re supposed to. But with patients doctors now becoming big brother, that statistic could change drastically.
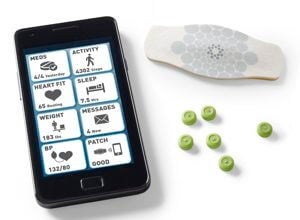
The device, made by Proteus Digital Health, is a silicon chip about the size of a sand particle. With no battery and no sensor, it is powered by the body itself. The chip contains small amounts of copper and magnesium. After being ingested the chip will interact with digestive juices to produce a voltage that can be read from the surface of the skin through a detector patch, which then sends a signal via mobile phone to inform the doctor that the pill has been taken. Sensors on the chip also detect heart rate and can estimate the patient’s amount of physical activity. More than just a way for doctors to look over their patients’ shoulders, it will allow doctors to better assess if a person is responding to a given dose, or if that dose needs to be adjusted.
After clinical trials that began in 2009, the FDA approval follows approval from European regulatory approval in August 2010. Right now the FDA has only approved the chip for placebo pills, which were used in trials showing the chip to be safe and highly accurate. Proteus hopes to gain approval to use the digestible chip with other medicines. Andrew Thompson, chief executive of Proteus, says the chip has already been tested with treatments for tuberculosis, mental health, heart failure, hypertension, and diabetes.
The company is currently working with makers of metformin, a drug used to treat type 2 diabetes and the most commonly prescribed drug in the world. The company also plans on adding a wireless glucose meter to their device so that dosage amount and frequency can be correlated with changes in blood glucose levels.
They would also like to digitize the drugs taken to treat neurological disorders. Disorders such as Parkinson’s Disease and Huntington’s Disease often require patients to receive drugs regularly – sometimes several times per day – and for extended periods of time. Ensuring that these patients are adhering to the prescribed regimen could greatly improve quality of life for some.

Transplant patients, who often have to take immunosuppressive drugs for long periods following surgery, could also potentially benefit from digitizing their medicine.
Ingestible body sensors have been discussed for a while now, but Proteus’ digital pills are the first ingestible sensor to be approved by the FDA, according to Nature. This first step toward regulated ingestible sensors will undoubtedly be followed by others. The Programmable Bio-Nano-Chip developed by Rice University scientists can detect heart disease or cancer from a saliva sample. If the chips were ever permanently implanted into the body, they could provide an early alarm system for these diseases long before symptoms are detected by the patient. Scientists at Tel Aviv University in Israel and Brigham & Women’s Hospital in Boston are developing a pill-sized robot that is remotely powered by an MRI machine to swim through the gut and look for the molecular signs of gastrointestinal cancer.
The first demonstration involved a placebo, but surely drug companies are eager to digitize their pills – and make sure patients empty out their prescriptions when they’re supposed to. Although possible, it is hard to imagine a complication would arise when the device is used with, say, Lipitor, that did not arise with the placebo. The usual FDA bottleneck could be loosened with the first incorporation into a bonafide drug.
The possible uses for ingestible sensors is as varied as the body itself. As with computer chips, ingestible chips will follow the exponential path of Moore’s Law and be able to sense more with less in the future. The FDA ruling could do much to get the technology on the fast track.
[image credits: Nature and Proteus Digital Health]
images: Nature and Proteus Digital Health



