A Brief Tour Through the Wild West of Neural Interfaces

Share
To most of us, zapping neurons with electricity to artificially “incept” memories, sensation, and movement still sounds crazy. But in some brain labs, that technology is beginning to feel old school. As a new review in Nature Biotechnology concludes: get off the throne, electrodes, there are plenty of other neural probes in town. They dance to the tune of light or chemicals, and in some cases, they’re bilingual.
Here’s a brief tour into the wild west of neural implants. Some require genetic engineering, and because of that have only been proven in experimental animals. But if history is any indication, brain-manipulation technologies don’t tend to stay in the lab. Watch out, you may see some trickling down into potential human use in the next few years.
What Makes a Good Implant, Anyway?
To be fair, electrodes are by far the most mature brain-interfacing technology. After all, our neurons mostly chit-chat using electrical “spikes” (with the help of some chemicals), which scientists have been able to measure and roughly decipher for decades. The logic is solid: an implanted electrode can “listen in” to record the neural chatter, and increasingly powerful software can help decode its signal, similar to cracking the Enigma code.
Once we know the code, delivering it back to the brain with electrical zaps should in theory reproduce that data in our biological wetware. When our internal code breaks—as in Alzheimer’s, major depression, or epilepsy—or is severed (in the case of paralysis), external input could patch up the nervous system’s information highway and restore function.
The problem, argued MIT professors Dr. James Frank, Marc-Joseph Antonini, and Polina Anikeeva, is we need to eventually move past classic implantable electrodes because they’re not specific enough. For one, they don’t target the types and groups of neurons needed to reproduce a thought or action. The result? Unwanted and unpredictable side effects.
For another, that’s not exactly how the brain works. Activity patterns in the brain occur at multiple resolutions—single neurons, neural networks, brain waves—and with different timing. It’s like trying to play a specific piano composition by reading sheet music: you have to hit the right notes and string them up at the correct strength and tempo, or the neural “song” will sound completely off.
The future of a successful brain probe, the authors said, is one that can integrate multiple levels of brain activity. The most straightforward way is to integrate multiple functions—electrical, light, chemical, magnetism—into a single probe. MiNDS (miniaturized neural drug delivery system), for example, can record from and chemically stimulate deep brain regions in non-human primates. For long-term implants, they also have to be soft and biocompatible with the brain to reduce scarring.
Finally, to truly link up brains to computers, they need to be “smart” closed-loop devices. Rather than zapping neurons based on a pre-programmed protocol, these smart implants measure brain activity and learn to only interfere when they detect anomalies. In this way, the implants are less likely to tamper with usual brain function—that is, they won’t screw up a person’s sense of self and control.
Light
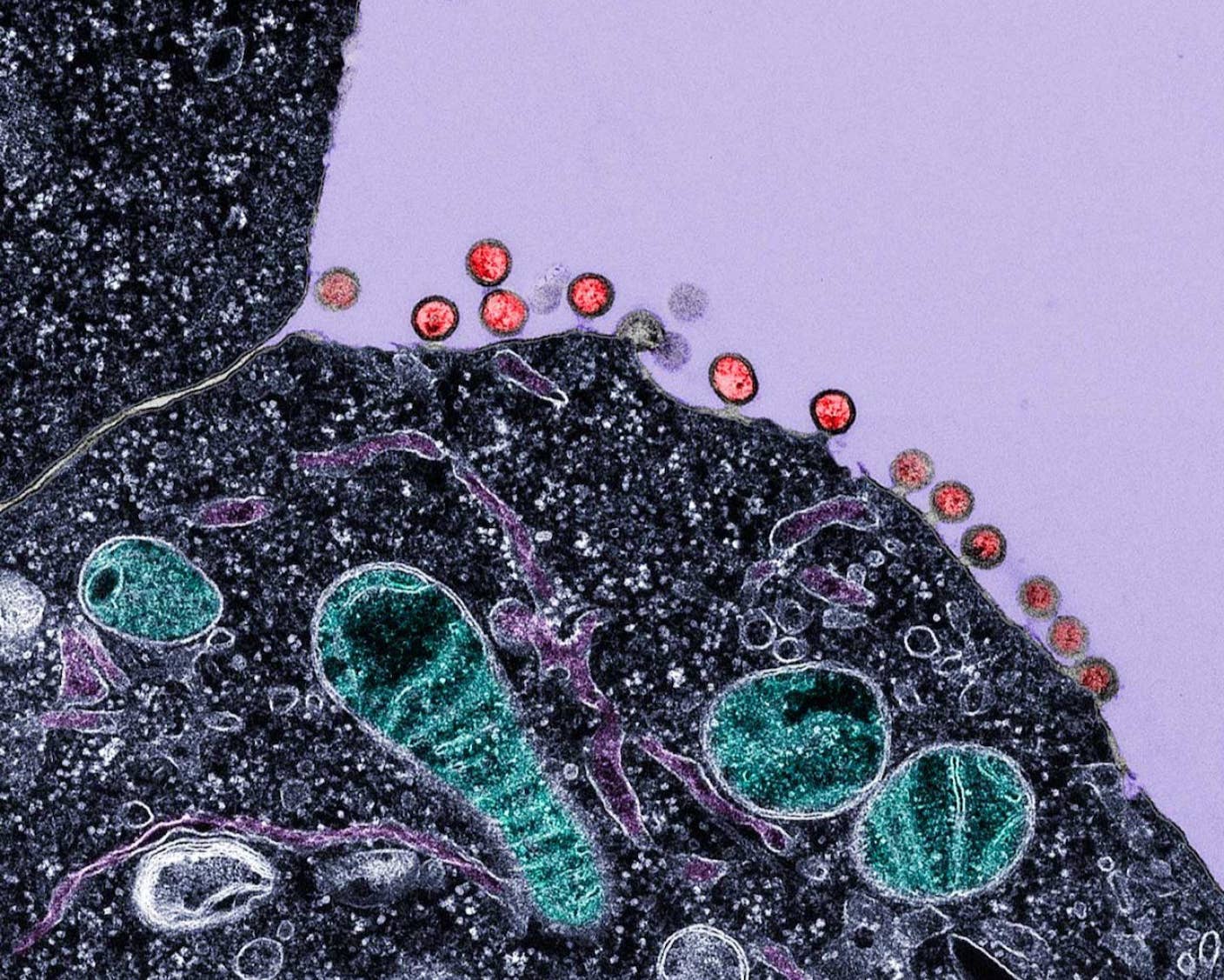
Optogenetics revolutionized neuroscience. Here, the trick is to genetically insert light-sensitive proteins, called opsins, into neurons. When triggered with light—blue is common, but you can almost use the entire rainbow—the proteins form a tunnel that lets ions rush in. That’s roughly how our neurons naturally fire, so light can act as an artificial trigger for activating or inhibiting specific neurons. Thanks to light, scientists have “written” artificial memories into mice or erased unwanted ones altogether.
Because the tool requires genetic engineering, so far the major push for clinical use is in blindness, since eyes are easy to access and naturally process light. Preliminary studies already found that natural light, through optogenetic proteins inside the retina, can help blind mice “see” and react to images similar to normal mice, though the proteins are less sensitive than the biological sensors in our eyes.
That said, scientists have been working hard to bring the elegant technique to human brains. One study this year “cut the cord,” developing a wireless, miniaturized optical implant that can be inserted under the scalp. Rather than batteries, the device was powered using external oscillating magnetic fields. The team could digitally control the intensity and frequency of the light and fine-tune neural activation.
Another study transformed existing optogenetics into near-infrared (NIR) wavelengths. Compared to blue light, NIR easily penetrates our skull and brain tissue without scattering, allowing it to reach deeper regions of the brain for modulation. A UC Berkeley team engineered nanoparticles into “light bulbs” that convert NIR light into traditional optogenetic blue-green light inside the brain. In this way, the team was able to activate neurons deep inside the mouse brain by shining NIR light from outside the skull, targeting neurons related to depression to release dopamine.
"We believe that achievements such as NIR…are rapidly unlocking numerous development routes and paving the way toward a bright therapeutic future," the authors said.
The yet unsolved problem is genetic engineering, and it’s not a simple one. Despite advances in genetic engineering, sticking gene-carrying viruses into the brain doesn’t sound super appealing to most. One study is hoping to convert light locally to heat, which then stimulates natural neurons without needing an extra gene (or two). Another idea is to first target the easier peripheral nervous system, making an optogenetic wireless implant that rests atop the spinal cord to reduce chronic pain. A prototype already exists for rodents, though the team is still working on implants for human use.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Chemical
No, we’re not talking about older-gen implants that flood the brain with chemicals, such as dopamine for Parkinson’s. Rather, chemicals are used in two main ways to control the brain: one, as designer drugs to specifically activate certain neurons, and two, as a combo with optogenetics to control neural circuits.
The first use case is kinda like optogenetics. Here, rather than sticking light-sensitive proteins into neurons, scientists stick designer proteins that open up into a channel only when a matching designer drug plops onto them. The technology, called DREADD (Designer Receptors Exclusively Activated by Designer Drugs) lets scientists multiplex their control over neural networks. More programming control? Way better understanding of how neurons unite to produce a behavior. Unfortunately, DREADDs also require genetically-altered neurons, and so far no one’s tried moving that tech to the clinics (yet). However, if we can leap over that giant hump, in theory you might be able to pop a pill or two and gain tailored control over specific neural circuits.
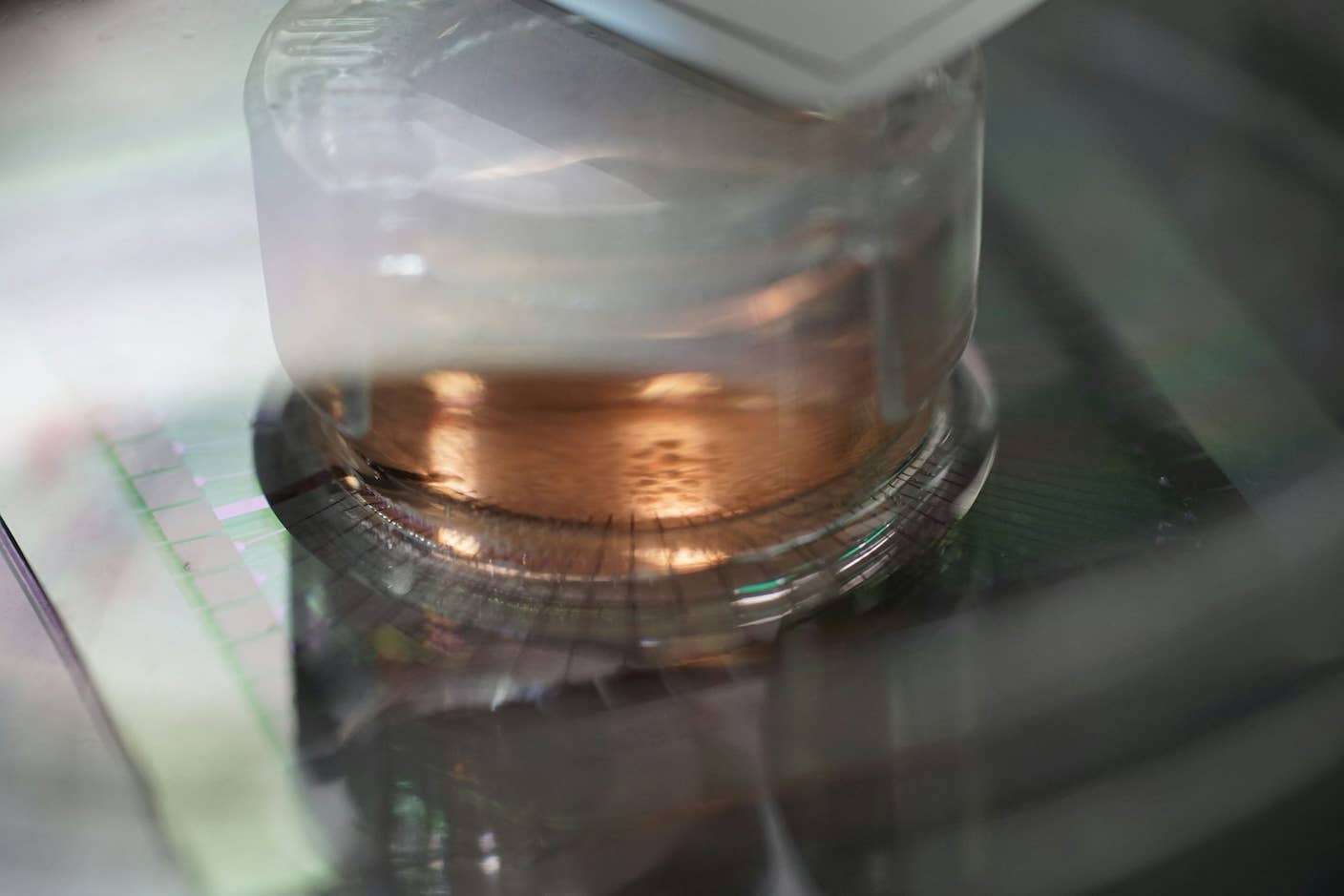
The second combo-hit is perhaps more exciting. A study this month combined drugs with optogenetics into a reloadable “optofluidic” probe. The squishy soft implant has a replaceable plug-like drug cartridge that can be reloaded for chronic chemical stimulation—dopamine is a favorite, since it’s implicated in depression, Parkinson’s, and movement, and light-stimulation on top helps reduce damage to neural tissues. The implant can be controlled wirelessly with a smartphone, is minimally invasive, and sucks up very little power. For now, the probe is used in animals to tease out neural network functions, but the team is interested in moving it towards the clinic.
Electricity
You’ve probably heard of the Walk Again Project, which uses brain implants such as the Utah Array to help paralyzed people regain movement in their off-line limbs. These microelectrodes use microfabrication techniques to make tiny silicon-based electrodes, and they’ve inspired newer-generation probes such as the Neuropixel, which packs nearly 1,000 recording sites along its 10mm shaft, about the size of five nickels stacked together.
That said, scientists have begun exploring soft, biocompatible electrodes to increase their implant lifespan. Because the brain and hard electrodes are mismatched in their mechanical properties, hard electrodes trigger an intense scarring reaction around the implant, which eventually renders it useless. The media-darling Neuralink, for example, uses jelly-fish-like soft, wispy electrodes that capture electrical activity from much smaller groups of neurons, and in theory should reduce the brain’s rejection response. Another idea, the Neural Lace, adopts a sandwich-like structure that allows it to flexibly conform to its host and integrate with brain tissues. In mice, the mesh could reliably stimulate the brain for eight months after implant.
One more example is Neurogrid, which uses biocompatible material at the electrode tip to reduce noise. A recent study found that these types of materials allow signal-carrying ions to more easily transport between the brain and the electrodes. Because the influx of ions is what makes neurons “fire,” it means that these materials are better suited for interfacing with our brains than standard silicon electrodes.
To the authors, the future is at least bi-modal. The transition of these new-generation electrical implants into clinics will provide more precise alternatives than what we currently have. But when paired with smart algorithms that allow closed-loop stimulation, and the reach of chemical and precision of optogenetics, we might finally be able to play our brains like musical instruments.
Image Credit: christitzeimaging.com / Shutterstock.com
Dr. Shelly Xuelai Fan is a neuroscientist-turned-science-writer. She's fascinated with research about the brain, AI, longevity, biotech, and especially their intersection. As a digital nomad, she enjoys exploring new cultures, local foods, and the great outdoors.
Related Articles

This Week’s Awesome Tech Stories From Around the Web (Through December 13)
New Immune Treatment May Suppress HIV—No Daily Pills Required
How Scientists Are Growing Computers From Human Brain Cells—and Why They Want to Keep Doing It
What we’re reading