This Group of Scientists Is Making Sure We’re Ready for the Next Pandemic
Share
Ask just about anyone how the US is doing on its response to the coronavirus pandemic and you’ll get some variation of the same answer: poorly. From a shortage of tests and medical supplies to mixed and contradictory official messaging to bureaucratic infighting, it’s clear we could have done better.
In fact, though a handful of countries displayed exemplary responses to the pandemic, the world as a whole was woefully unprepared for the reality we’re now living in. To be fair, no one saw this coming (except maybe Bill Gates), and it was easy to ignore a hypothetical-but-seemingly-unlikely threat when we had plenty of other problems on our hands.
Though it’s too late to save us this time around, new pandemic-fighting movements are springing up all over the world. One of the most comprehensive of these was announced last week: led by Harvard Medical School, the Massachusetts Consortium on Pathogen Readiness will use a $115 million research grant to help fight Covid-19 and to prepare the world for future pandemics, in partnership with China’s Guangzhou Institute of Respiratory Health.
The consortium is focusing its efforts on six distinct areas of study. Here’s what you should know about each one.
Epidemiology
Epidemiologists use data to predict and monitor the spread of disease, looking at factors like severity, transmission rate, and evolution of a pathogen over time.
The consortium’s epidemiology group will focus on gathering granular raw data at various levels, from whole countries and states down to specific workplaces and households; predictive models of Covid-19’s spread will be more accurate and reliable the more data they can pull in. Are people obeying social distancing orders? Is it working? Once the virus hits a new city, how many people are likely to need hospitalization within a week? Two weeks?
It’s pretty amazing how far some good data can get us; having accurate answers to these questions before urgency sets in means we’ll have an inkling of what’s coming rather than flailing helplessly amid chaos—and we’ll be able to get resources like masks, tests, and ventilators to where they’re about to be needed most (though admittedly, actually having these resources on hand is a whole other issue).
Diagnostics
One of the big coronavirus flubs we’ve had in the US is our lack of widespread testing and diagnostics. Even people with Covid-19-like symptoms who show up at hospitals have been turned away without a test if they’re not elderly or haven’t knowingly come into contact with an infected person. If we were testing more people—even those with no symptoms—we’d know who was safe to go back to work rather than needing to do blanket lockdowns across the country.
The consortium’s diagnostics division will work on three different types of tests, all of which they feel are crucial to overcoming the pandemic. Ultra-sensitive assays could detect coronavirus even at very low levels and would have a turnaround time as quick as 30 minutes. Critical disease biomarker tests would identify people at higher risk of becoming critically ill due to pre-existing conditions or other factors. And antibody tests will indicate the people who’ve had the virus (possibly without ever feeling sick), recovered, and are now immune—more on these below.
Pathogenesis
How, exactly, does Covid-19 interact with our bodies and immune systems? It’s sort of like SARS and MERS, but one of the biggest and most sinister differences is the way a newly-infected person can be carrying Covid-19 for days without showing any symptoms—and thus unknowingly spreading it to others. Why are some people silent carriers while others end up in the ER? And in the latter group, how does the virus cause so much inflammation in the respiratory system?
The pathogenesis group will be working to find answers to these and other complex questions around how Covid-19 invades and takes over our healthy cells. One key is to figure out which immune signaling pathways are induced to trigger an abnormal immune response in the human body, as well as whether recovering from the virus bestows long-lasting immunity on someone or if the virus can mutate and re-infect the same host.
Clinical Disease Management
Developing a Covid-19 vaccine is going to take a year at best. In the meantime, we can use existing antiviral medicines to help people survive the virus.
You’ve probably heard of chloroquine by now. It’s one of a few drugs scientists are trying to repurpose for use against Covid-19 and it’s already in clinical trials in multiple countries, as is an Ebola drug called remdesivir. Besides being readily available, existing drugs are a good option because we already know their safety profiles, effective dosages, and side effects. Researchers will also use computer-based screening to look for molecules that might bind to the novel coronavirus’s target protein.
“Our current efforts are focused on what we can do now, but I think we want to keep an eye on what we can build so the next time this happens we're in a place where we can react more rapidly,” said Mark Namchuk, who co-leads this group.
Be Part of the Future
Sign up to receive top stories about groundbreaking technologies and visionary thinkers from SingularityHub.


Therapeutics
Developing an antibody treatment isn’t fast or cheap; it requires extraction and purification of blood plasma from recovered patients, followed by testing and transfusion into sick people. The biggest challenge of such a treatment for this coronavirus is finding the right antibodies to disable the virus.
Wayne Marasco, an immunologist-oncologist with training in infectious diseases, Harvard med school professor, and member of the consortium’s treatment working group, was actively involved in the SARS and MERS outbreaks of 2003-2012—and he’s been building a vast library of human antibodies for over 20 years, with the current count at 27 billion.
Marasco pointed out that if two different coronaviruses can jump from animals to humans within less than 20 years of one another, it's only a matter of time before another jump occurs. “These viruses have the ability to jump species by just an accidental mutation and, given the vector and the right exposure, that could be enough,” he said. “We have to be proactive and assume that there are continuous zoonotic transfers.”
Vaccines
A Covid-19 vaccine, of course, is what we’re all holding our breaths for—it’s the thing that will truly mean this pandemic is over (and boy do we want this pandemic to be over).
Though we are, as mentioned, likely at least a year away from a vaccine, the team points out three reasons for optimism. First, Covid-19’s mortality rate is low; most people who get the virus recover, which indicates the pathogen may induce natural immunity. Second, the virus hasn’t mutated from its initial form as of yet, which means a single vaccine may be effective against it. Third, the spike protein the virus uses to enter and infect human cells is a clear target for a vaccine.
Two vaccine candidates are already in development in Dan Barouch’s lab, co-leader of the consortium's vaccine development arm. And check out this timeline and tell me if isn’t impressive: the SARS-CoV-2 sequence was released on January 10th. By the 13th, Barouch's lab had ordered synthetic viral genes for two vaccine platforms. On Jan. 31st, they entered a collaboration with Johnson & Johnson to develop a Covid-19 vaccine. By February 6th they had immunized the first mice, and they’re aiming to start clinical trials in humans in the fall.
Building the Arsenal
It’s becoming clearer that even once this pandemic is over and we can all return to something resembling our normal lives, the world isn’t going back to how it was in 2019. There will be some big changes in how we travel, interact, and do business.
But, if maybe less than before, people will still travel. International trade will continue. Supply chains will still go through multiple countries. And in the midst of all this, the global population will continue to grow, with cities that are already densely populated becoming denser still.
We live in an irrevocably globalized world, and Covid-19 is not the last global-scale pandemic we will face; there will be more. We don’t yet know what they’ll look like; maybe the next virus will have a higher transmission rate but a lower mortality rate, or vice versa—but projects like the Massachusetts Consortium are making sure that whatever comes our way, we’ll be ready for it.
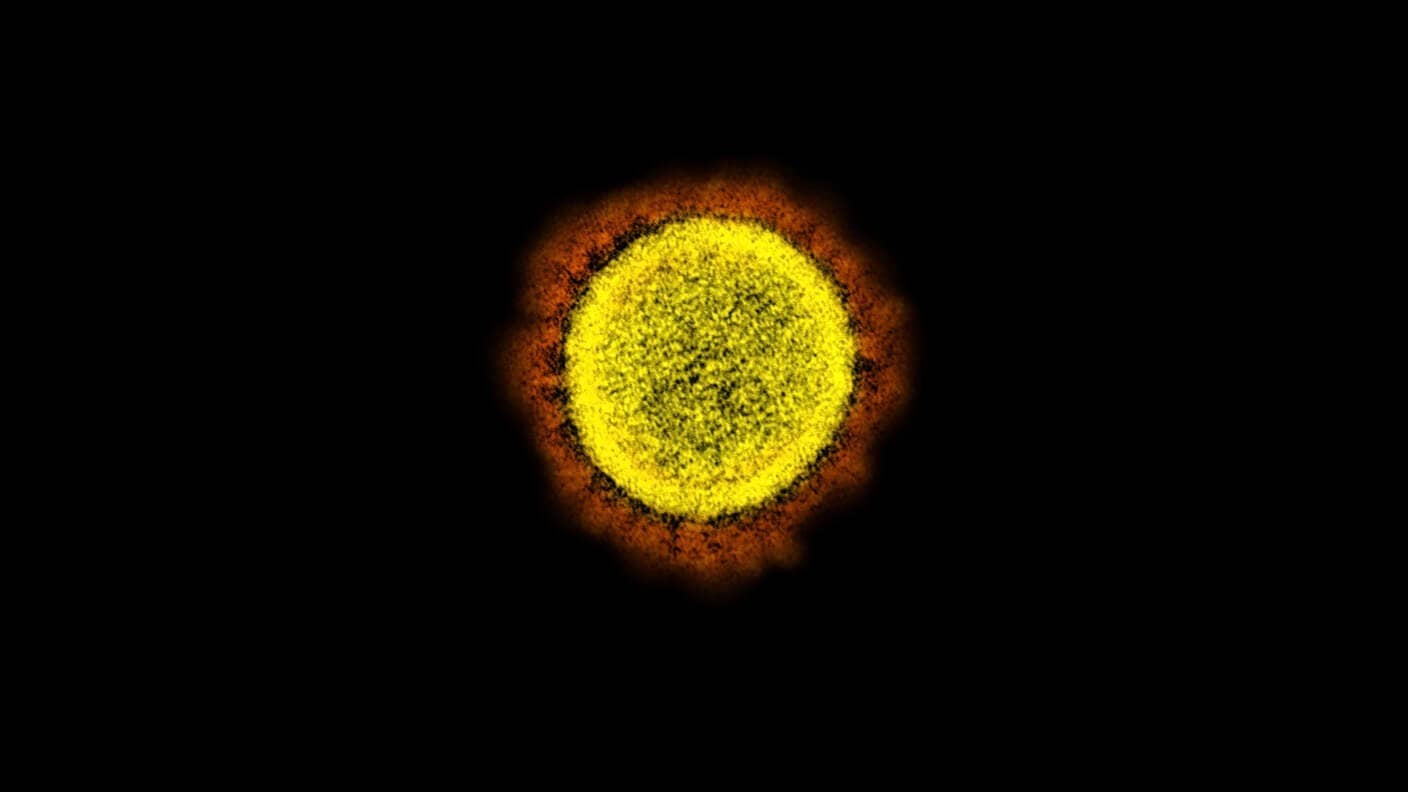
Image Credit: SARS-CoV-2 virus particle / NIH
Vanessa has been writing about science and technology for eight years and was senior editor at SingularityHub. She's interested in biotechnology and genetic engineering, the nitty-gritty of the renewable energy transition, the roles technology and science play in geopolitics and international development, and countless other topics.
Related Articles

Souped-Up CRISPR Gene Editor Replicates and Spreads Like a Virus

Your Genes Determine How Long You’ll Live Far More Than Previously Thought

Google DeepMind AI Decodes the Genome a Million ‘Letters’ at a Time
What we’re reading